If you’re experiencing constipation while taking calcium channel blockers, adjusting your diet can provide relief. Incorporating high-fiber foods such as fruits, vegetables, and whole grains into your meals is a simple yet effective strategy. Aim for at least 25-30 grams of fiber each day to support healthy digestion and bowel regularity.
Hydration plays a key role as well. Drinking sufficient water helps soften the stool and facilitates its passage. Aiming for eight 8-ounce glasses of water daily can promote gastrointestinal health. Additionally, consider adding regular physical activity to your routine, as exercise stimulates bowel function.
Consult your healthcare provider if constipation persists despite these self-care measures. They may recommend adjusting your medication or suggest specific over-the-counter remedies. It’s important to manage this side effect effectively to maintain your overall wellbeing while on calcium channel blockers.
- Calcium Channel Blockers and Constipation
- Understanding Calcium Channel Blockers
- Mechanism of Action and Its Effects on the Body
- Impact on Smooth Muscle
- Cardiac Effects
- Common Calcium Channel Blockers and Their Uses
- Types of Calcium Channel Blockers
- Clinical Applications
- Link Between Calcium Channel Blockers and Gastrointestinal Motility
- Prevalence of Constipation in Patients Taking Calcium Channel Blockers
- Symptoms and Diagnosis of Constipation Related to Medication
- Management Strategies for Constipation Induced by Calcium Channel Blockers
- Physical Activity
- Medications and Supplements
- Patient Education and Counseling on Medication Side Effects
Calcium Channel Blockers and Constipation
Calcium channel blockers (CCBs) can lead to constipation in some patients. This side effect is due to the relaxation of smooth muscle in the gastrointestinal tract caused by the medication. If you’re experiencing constipation while on a CCB, consider adjusting your diet to include more fiber-rich foods such as fruits, vegetables, and whole grains. Increasing water intake is also beneficial, as staying hydrated helps to soften stool and promote regular bowel movements.
Regular physical activity can stimulate intestinal motility and alleviate constipation symptoms. Aim for at least 30 minutes of moderate exercise most days of the week. If lifestyle changes do not help, discuss with your healthcare provider the option of using a gentle laxative or stool softener to relieve symptoms.
If constipation persists, your doctor may evaluate your medication regimen. They may consider switching to another antihypertensive drug that has a lower risk of causing constipation. Always consult with your healthcare provider before making any changes to your medication or treatment plan.
Monitor your symptoms closely. Keeping a journal of your dietary habits and bowel movements can provide valuable insight when discussing your concerns with your healthcare professional. With proper management, it’s possible to minimize the impact of CCB-induced constipation on your daily life.
Understanding Calcium Channel Blockers
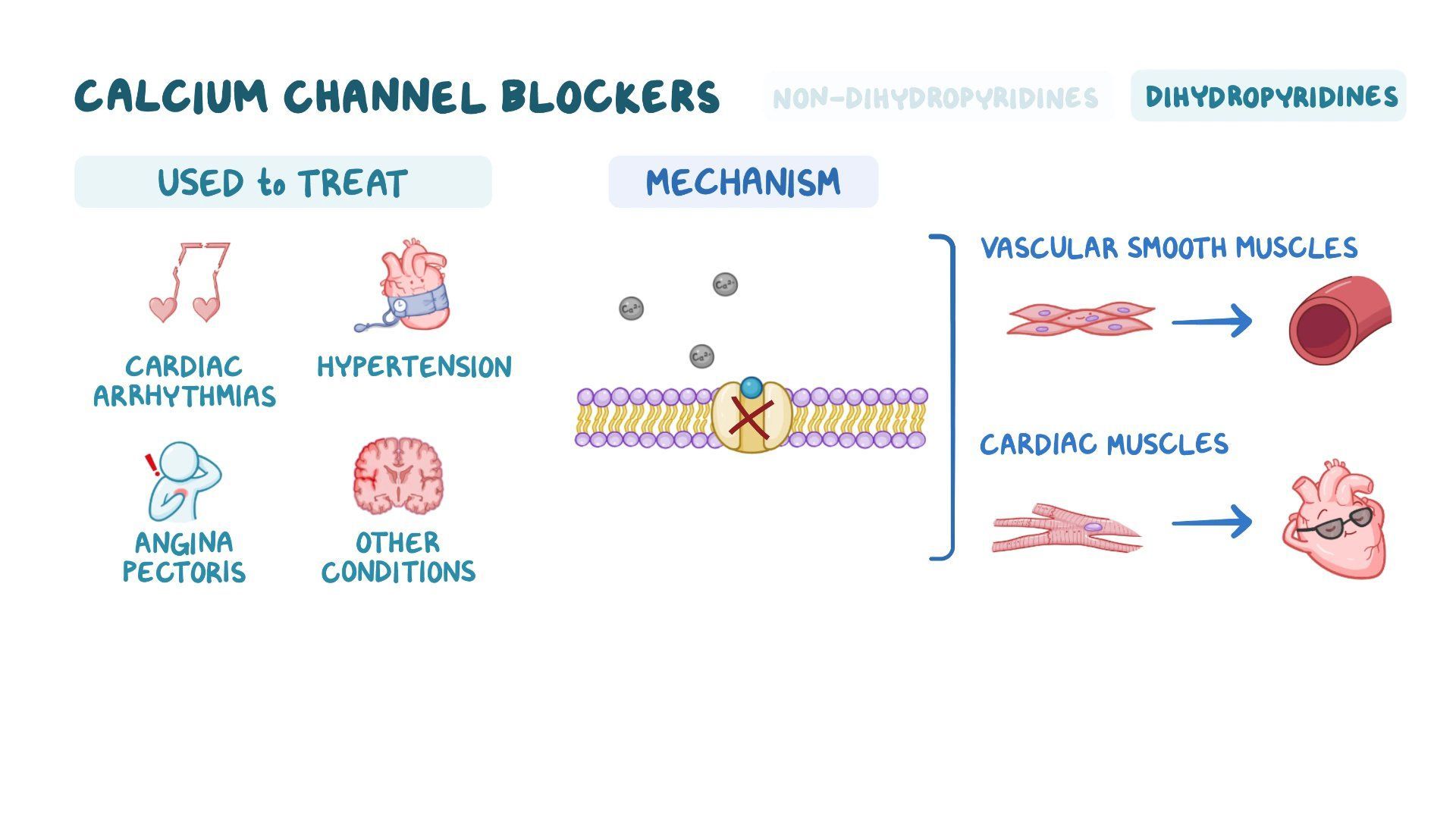
Calcium channel blockers (CCBs) play a crucial role in managing cardiovascular conditions. These medications primarily relax blood vessels, improving blood flow and reducing blood pressure. They target calcium channels on the cells of the heart and blood vessels, inhibiting calcium’s entry and leading to muscle relaxation.
Common types of calcium channel blockers include:
- Dihydropyridines: Such as amlodipine and nifedipine, primarily affecting blood vessels.
- Non-dihydropyridines: Such as diltiazem and verapamil, affecting both the heart and blood vessels.
In addition to hypertension, CCBs help treat conditions like angina and certain types of arrhythmias. Their action results in decreased heart rate and improved oxygen delivery to the heart muscle, beneficial for patients with coronary artery disease.
However, calcium channel blockers can cause side effects. A notable one is constipation, particularly with non-dihydropyridines. Those experiencing this should consider the following strategies:
- Increase dietary fiber: Incorporate fruits, vegetables, and whole grains into meals.
- Stay hydrated: Drink plenty of water throughout the day to facilitate digestion.
- Regular exercise: Physical activity can stimulate bowel function and alleviate constipation.
Monitoring is key. Patients using CCBs should consult their healthcare provider if constipation becomes persistent, as adjusting medication or implementing specific dietary changes may be necessary for relief.
Understanding the mechanism and managing side effects effectively can enhance the overall treatment experience for individuals on calcium channel blockers.
Mechanism of Action and Its Effects on the Body
Calcium channel blockers (CCBs) function by inhibiting the influx of calcium ions through L-type calcium channels located in the smooth muscle and cardiac tissue. This mechanism creates a series of physiological effects that influence various systems in the body.
Impact on Smooth Muscle
By blocking calcium entry, CCBs relax vascular smooth muscle, leading to:
- Reduced vascular resistance
- Lowered blood pressure
- Improved coronary blood flow
This relaxation effect extends to other smooth muscle tissues, including the gastrointestinal (GI) tract, contributing to a slower motility and potential constipation.
Cardiac Effects
In the heart, reducing calcium influx affects the following:
- Decreased heart rate
- Reduced contractility
- Prolonged conduction time through the AV node
These effects help manage conditions like hypertension and arrhythmias, but can also play a role in overall energy levels and physical activity due to decreased cardiac output during certain times.
Understanding the effect of calcium channel blockers on smooth muscle and cardiac function provides a clearer picture of why some patients may experience constipation as a side effect. Monitoring these symptoms and adjusting medication if necessary can enhance patient comfort and quality of life.
Common Calcium Channel Blockers and Their Uses
Calcium channel blockers (CCBs) play a significant role in managing various cardiovascular conditions. They relax blood vessels, reduce heart workload, and lower blood pressure. Here are some commonly prescribed CCBs and their therapeutic applications.
Types of Calcium Channel Blockers
The two main categories of CCBs are dihydropyridines and non-dihydropyridines. Dihydropyridines primarily target the peripheral vascular system, while non-dihydropyridines affect both the heart and blood vessels.
| Medication | Classification | Primary Uses |
|---|---|---|
| Amlodipine | Dihydropyridine | Hypertension, angina |
| Nifedipine | Dihydropyridine | Hypertension, angina, Raynaud’s phenomenon |
| Verapamil | Non-Dihydropyridine | Hypertension, angina, atrial fibrillation |
| Diltiazem | Non-Dihydropyridine | Hypertension, angina, atrial fibrillation |
Clinical Applications
Amlodipine is frequently chosen for its once-daily dosing and effectiveness in hypertension. Nifedipine, with its rapid action, is useful in acute scenarios such as hypertensive crises. Verapamil and Diltiazem are often selected for patients with arrhythmias, providing both rate control and blood pressure reduction.
Regular monitoring is necessary, as these medications may lead to side effects like constipation. Patients should stay informed and communicate with healthcare providers regarding their experiences.
Link Between Calcium Channel Blockers and Gastrointestinal Motility
Calcium channel blockers (CCBs) can significantly affect gastrointestinal motility, potentially leading to constipation. These medications relax smooth muscles, including those in the gastrointestinal tract. This relaxation may result in decreased peristalsis, the wave-like motion that moves food through the intestines.
Many patients on CCB therapy report symptoms of constipation. Here are some key points regarding this relationship:
- Mechanism of Action: CCBs inhibit calcium entry into cells, reducing muscle contraction strength. Smooth muscles in the gut do not contract effectively, resulting in slower transit times.
- Types of CCBs: Dihydropyridine CCBs, such as amlodipine, are more likely to cause constipation compared to non-dihydropyridine types like verapamil, which can also have a direct constipating effect.
- Prevalence: Studies indicate that up to 30% of patients using CCBs may experience constipation symptoms.
- Management Strategies: Increase dietary fiber intake, ensure adequate hydration, and consider the addition of exercise to help mitigate constipation effects.
- Alternative Medications: If constipation becomes problematic, healthcare providers may evaluate the need for alternative antihypertensive agents without constipating effects.
Awareness of these effects guides healthcare professionals and patients in addressing gastrointestinal issues that may arise during CCB therapy. Utilizing lifestyle modifications can alleviate symptoms and enhance overall comfort while maintaining treatment efficacy.
Prevalence of Constipation in Patients Taking Calcium Channel Blockers
Current research indicates that constipation affects approximately 10-30% of patients using calcium channel blockers (CCBs). This side effect often arises due to the drug’s impact on smooth muscle contraction in the gastrointestinal tract. As CCBs relax vascular smooth muscle to lower blood pressure, they can inadvertently reduce motility in the intestines, contributing to constipation.
A study found that patients on CCB therapy experienced a twofold increase in reports of constipation compared to those not taking these medications. Among different classes of CCBs, the frequency of constipation varies; dihydropyridines, such as amlodipine, tend to have a higher incidence compared to non-dihydropyridines like verapamil.
Patients who report gastrointestinal issues should regularly assess their bowel habits and drink plenty of fluids. Increasing dietary fiber can alleviate symptoms for many. Physical activity also plays a significant role in promoting regularity. In some cases, healthcare professionals may recommend adjusting the medication regimen or prescribing laxatives to manage severe constipation effectively.
Monitoring and addressing constipation in patients taking CCBs is essential for improving quality of life and adherence to treatment. Regular follow-ups and open communication with healthcare providers help in optimizing management strategies tailored to individual needs.
Symptoms and Diagnosis of Constipation Related to Medication
Identify key symptoms associated with medication-induced constipation. Common indicators include infrequent bowel movements, straining during defecation, abdominal discomfort, and hard or lumpy stools. Patients may also experience a sensation of incomplete evacuation after a bowel movement.
Monitoring the frequency of bowel movements can provide insights. Most healthy adults typically have at least three bowel movements per week. A noticeable decrease can signal constipation, particularly when it persists for several days.
Diagnosis often begins with a thorough patient history. Healthcare providers assess any recent changes in medication, diet, or lifestyle. Discussing the timing of constipation in relation to new medications can offer clues about causation. Physicians may also perform a physical examination, focusing on abdominal and rectal areas to identify any underlying issues.
Diagnostic tests, like X-rays or colonoscopy, may be recommended if symptoms persist or worsen. These tests check for obstructions or abnormalities in the digestive tract. Stool tests can evaluate the presence of blood or infections, ruling out other potential causes of constipation.
Consider lifestyle modifications alongside medication reviews. Increasing water intake and dietary fiber can alleviate symptoms. Regular physical activity also promotes gut health, mitigating constipation risks. Collaboration between patients and healthcare providers ensures a comprehensive approach to diagnosing and managing medication-related constipation.
Management Strategies for Constipation Induced by Calcium Channel Blockers
Incorporate dietary changes to enhance bowel movements. Increase fiber intake by adding fruits, vegetables, whole grains, and legumes to meals. Aim for a daily fiber goal of 25-30 grams to help improve stool consistency and promote regularity.
Stay well-hydrated. Drinking sufficient water, approximately 8-10 glasses daily, aids in softening stool. Herbal teas, especially those with a mild laxative effect, can also be beneficial.
Physical Activity
Engage in regular exercise. Activities such as walking, jogging, or yoga stimulate intestinal motility. Aim for at least 150 minutes of moderate exercise weekly to naturally encourage bowel function.
Medications and Supplements
Consider over-the-counter options like stool softeners or laxatives if dietary and lifestyle changes are insufficient. Options like polyethylene glycol (MiraLAX) can effectively relieve constipation. Consult with a healthcare provider before starting any medication.
| Strategy | Description |
|---|---|
| Increase Fiber | Include fruits, vegetables, whole grains in diet. |
| Stay Hydrated | Drink 8-10 glasses of water daily. |
| Regular Exercise | 150 minutes of physical activity weekly. |
| Use Medications | Consider stool softeners or laxatives as needed. |
Monitor your response to these strategies. Adjust dietary and lifestyle alterations based on individual experiences. Consult healthcare professionals if constipation persists or worsens, ensuring a tailored approach to management.
Patient Education and Counseling on Medication Side Effects
Discuss the possibility of constipation as a side effect of calcium channel blockers with your patients. Encourage them to monitor their bowel habits closely while on these medications.
Suggest incorporating more fiber into their diet by eating fruits, vegetables, and whole grains. Recommend drinking plenty of fluids, aiming for at least 8 glasses of water a day to help maintain regular bowel movements.
Advise patients to engage in regular physical activity, as even moderate exercise can promote digestive health and alleviate constipation. Simple activities like walking or gentle stretching can be beneficial.
If constipation occurs, recommend over-the-counter options such as fiber supplements or mild laxatives. Encourage patients to seek medical advice if constipation persists for more than a few days or if they experience significant discomfort.
Reassure patients that they should not stop taking their medication without consulting their healthcare provider. Discuss potential alternatives or adjustments to dosage if constipation becomes a major issue.
Provide written materials summarizing these suggestions, and invite patients to ask questions during their appointments. Creating an open line of communication helps ensure they feel supported in managing their side effects.