Clarithromycin and azithromycin belong to the macrolide antibiotic class and are frequently used to treat various bacterial infections. While they share similar applications, these medications have distinct properties and pharmacokinetics that set them apart.
Clarithromycin tends to have a longer half-life compared to azithromycin, allowing for potentially shorter treatment regimens. It is often chosen for respiratory infections and certain skin conditions due to its broader spectrum against specific bacteria.
Azithromycin, on the other hand, is favored for its convenient dosing schedule and is commonly prescribed for respiratory infections, sexually transmitted infections, and even for certain gastrointestinal bacterial infections. Its ability to penetrate well into tissues makes it particularly effective for conditions like pneumonia.
While both antibiotics are effective against similar pathogens, the choice between clarithromycin and azithromycin often depends on the specific infection being treated, patient tolerance, and local resistance patterns. Always consult a healthcare professional to determine the most appropriate option for your condition.
Clarithromycin and Azithromycin: Understanding Their Differences
Clarithromycin and azithromycin are widely used antibiotics, but they exhibit distinct characteristics. Clarithromycin typically requires a longer treatment course, often two weeks, due to its pharmacokinetics. Azithromycin, on the other hand, has a shorter dosing schedule, commonly lasting about five days, which can enhance patient compliance.
Clarithromycin displays a broader spectrum of activity against certain bacteria, particularly some strains of respiratory pathogens. It may be preferred for treating infections like community-acquired pneumonia. Azithromycin excels against a variety of infections too, but it shines in treating atypical pathogens and sexually transmitted infections due to its unique mechanism of action.
Side effects differ between the two medications. Clarithromycin is more likely to cause gastrointestinal disturbances and has a higher potential for drug interactions due to its effect on liver enzymes. Azithromycin generally has a milder side effect profile and poses fewer drug interaction risks, making it a more convenient option for many patients.
When considering their usage, it is important to take into account any specific bacterial susceptibility, patient history, and the potential for resistance. Always consult with a healthcare professional to determine which antibiotic is the most suitable for your particular situation.
Comparative Efficacy of Clarithromycin and Azithromycin in Treating Bacterial Infections
Clarithromycin and azithromycin both show significant effectiveness against various bacterial infections. Clarithromycin excels in treating respiratory tract infections, particularly those caused by Streptococcus pneumoniae and Haemophilus influenzae. Its ability to penetrate respiratory tissues effectively enhances its performance in managing pneumonia and bronchitis.
Azithromycin, on the other hand, is highly effective for atypical bacteria and is often the first choice for managing infections caused by Mycoplasma pneumoniae and Chlamydia pneumoniae. Beyond respiratory issues, azithromycin also treats sexually transmitted infections, such as chlamydia, with great success due to its prolonged tissue half-life.
Pharmacokinetics and Dosing
Clarithromycin requires twice-daily dosing, which may affect patient adherence. Azithromycin, with its once-daily regimen and extended half-life, often improves compliance. Healthcare providers can consider these factors when prescribing, especially in outpatient settings where adherence is critical to treatment success.
Side Effects and Considerations
Clarithromycin may cause gastrointestinal side effects, such as nausea and diarrhea, which could deter some patients. Azithromycin generally has a milder side effect profile, making it a preferred choice in pediatric and sensitive populations. However, monitoring for potential cardiovascular effects, particularly in patients with existing heart conditions, is essential when using azithromycin.
This comparative analysis of clarithromycin and azithromycin highlights their unique strengths in treating bacterial infections. Clinicians should tailor their choice based on the specific infection, patient tolerance, and dosing convenience to optimize treatment outcomes.
Dosage, Side Effects, and Considerations for Using Clarithromycin vs. Azithromycin
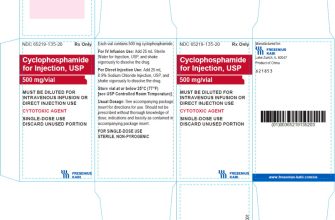
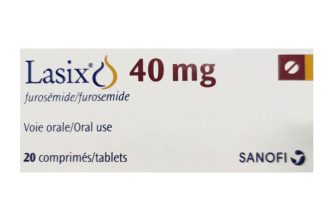
For adults, the typical dosage of Clarithromycin ranges from 250 mg to 500 mg every 12 hours, depending on the severity of the infection. The course usually lasts from 7 to 14 days. Azithromycin, on the other hand, is often prescribed in a loading dose of 500 mg on the first day, followed by 250 mg daily for the next 4 days, totaling a common regimen of 5 days. Adjustments may be needed for renal function, particularly with clarithromycin.
Side effects can differ between the two medications. Clarithromycin may lead to gastrointestinal issues like diarrhea and nausea, along with possible metallic taste. Rarely, it can cause liver toxicity and QT prolongation. Azithromycin is usually better tolerated but can also cause gastrointestinal discomfort and has been associated with cardiovascular risks in certain populations. Both can provoke allergic reactions, so monitoring for signs of rash or swelling is critical.
Considering drug interactions is essential for both antibiotics. Clarithromycin is known for significant interactions due to its effect on CYP450 enzymes, which can increase the concentrations of many concurrent medications. Azithromycin has a lower potential for interactions, making it a safer option for patients on polypharmacy.
Evaluate patient-specific factors such as age, renal function, and any existing health conditions. Pregnant individuals should consult healthcare providers before use, as both medications carry potential risks. Discussing treatment goals and medication adherence is vital in optimizing outcomes for infections.