Yes, Lasix can lead to sodium depletion. As a diuretic, it promotes the excretion of sodium through urine, which can result in decreased sodium levels in the body if not managed properly. Patients taking Lasix should be aware of this potential side effect and monitor their electrolyte levels regularly.
Maintaining a balanced electrolyte level is crucial for overall health. Sodium plays a significant role in fluid balance, muscle function, and nerve signaling. Therefore, if you are prescribed Lasix, consider incorporating sodium-rich foods into your diet or discussing sodium supplementation with your healthcare provider, especially if you experience symptoms like dizziness, muscle cramps, or fatigue.
Regular check-ups can help track your sodium levels while on Lasix. Staying informed about dietary adjustments and recognizing signs of sodium depletion can lead to better management of your condition. Always consult with your doctor before making any changes to your treatment or diet to ensure safe and effective care.
- Does Lasix Deplete Sodium?
- Understanding Lasix: Mechanism of Action
- Clinical Implications of Sodium Depletion
- Symptoms and Management
- Long-term Considerations
- Monitoring Sodium Levels While on Lasix
- Signs of Sodium Depletion
- Maintaining Sodium Balance
- Management Strategies for Sodium Depletion
- Hydration Considerations
- Regular Monitoring
- Patient Education on Lasix and Sodium Balance
Does Lasix Deplete Sodium?
Yes, Lasix (furosemide) can deplete sodium levels in the body. This diuretic promotes increased urine production, leading to the excretion of excess fluids and electrolytes, including sodium. Monitoring sodium levels during treatment is essential.
If you are prescribed Lasix, it’s crucial to discuss your sodium intake with your healthcare provider. Adjusting your diet to include appropriate levels of sodium can help manage potential depletion. Foods rich in sodium, such as table salt, canned soups, and processed foods, can be beneficial, but consult your doctor before making significant dietary changes.
Be vigilant for signs of sodium depletion, which may include dizziness, confusion, muscle cramps, and fatigue. If you notice these symptoms, reach out to your healthcare professional immediately to evaluate your condition and consider adjustments to your treatment plan.
Regular check-ups and blood tests are recommended to monitor your electrolyte levels while on Lasix. This proactive approach helps ensure your sodium levels remain within a healthy range and minimizes potential complications.
In summary, Lasix does deplete sodium, and proactive management of your sodium intake and monitoring can mitigate risks associated with this effect.
Understanding Lasix: Mechanism of Action
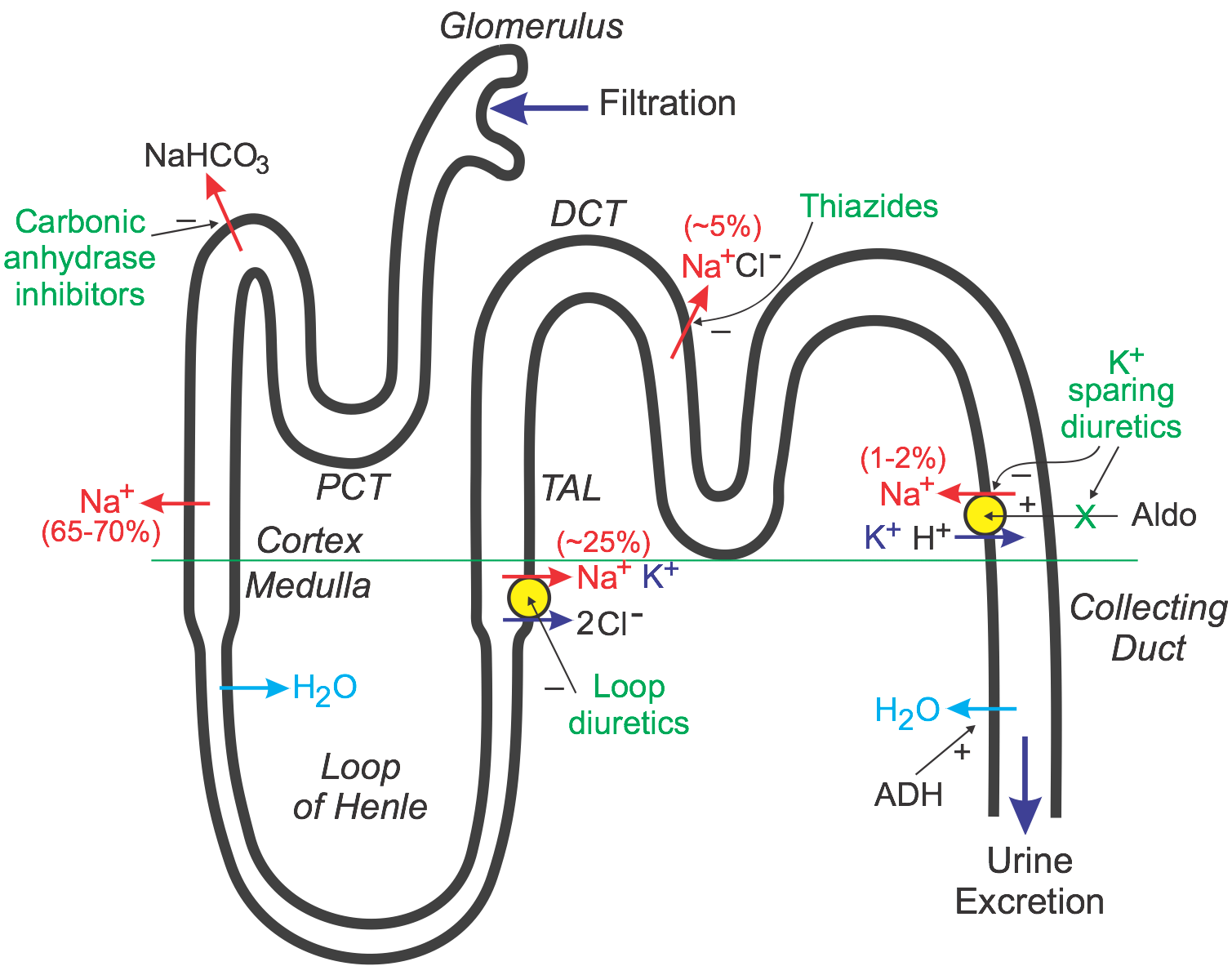
Lasix, known scientifically as furosemide, operates primarily as a loop diuretic. It functions by inhibiting sodium and chloride reabsorption in the ascending loop of Henle within the kidneys. This action leads to increased urine output, effectively promoting the excretion of excess fluid and electrolytes from the body.
The blockage of the Na-K-2Cl transporter reduces the reabsorption of these ions, causing a significant amount of sodium to be excreted in the urine. As a result, not only sodium is lost, but also water follows osmotically, leading to diuresis. This mechanism is particularly beneficial in conditions like heart failure, where excess fluid accumulation occurs.
Patients receiving Lasix may notice increased urination shortly after administration, reflecting the rapid onset of its action. Monitoring electrolyte levels, particularly sodium, is advisable during treatment, as continued use can lead to depletion and other imbalances.
In addition to sodium, potassium levels may also decrease. Combining Lasix with potassium-sparing diuretics or potassium supplements can help mitigate this risk, ensuring patients maintain proper electrolyte balance.
Understanding the mechanism of Lasix allows for better management of its effects and potential side effects. Regular follow-ups and laboratory tests assist in maintaining optimal health while using this medication.
Clinical Implications of Sodium Depletion
Healthcare providers should monitor sodium levels in patients on Lasix, particularly those with underlying conditions such as heart failure or renal impairment. Regular checks help prevent complications associated with hyponatremia.
Symptoms and Management
Sodium depletion can manifest as headache, confusion, weakness, and muscle cramps. Recognizing these symptoms early allows for prompt management. Adjusting the dose of Lasix or administering supplemental sodium can effectively mitigate risks.
Long-term Considerations
Chronic sodium depletion may lead to additional complications, including increased risk of falls and cardiovascular events. Employing a diet rich in sodium or discussing medication alternatives with patients aids in maintaining optimal levels. Regular follow-up appointments to assess both sodium levels and overall health are essential.
Monitoring Sodium Levels While on Lasix
Regularly check sodium levels while taking Lasix to prevent hyponatremia. Aim for routine blood tests every one to two weeks initially, gradually extending the interval to monthly as stabilization occurs.
Signs of Sodium Depletion
Watch for symptoms such as headache, nausea, confusion, or muscle cramps. These may indicate low sodium levels. If any of these appear, consult a healthcare provider promptly for assessment.
Maintaining Sodium Balance
Include sodium-rich foods in your diet if allowed by your healthcare provider. Foods like table salt, pickles, olives, and broth can help maintain adequate levels. Hydration remains important; however, balance fluid intake with sodium needs as guided by a healthcare professional.
| Action | Frequency |
|---|---|
| Blood tests for sodium levels | Every 1-2 weeks initially |
| Consult healthcare provider for symptoms | As needed |
| Review dietary sodium intake | Monthly |
Management Strategies for Sodium Depletion
Increase dietary sodium intake by adding salt to your meals or consuming sodium-rich foods like pickles, olives, and processed snacks. Monitor your total daily sodium consumption, aiming for a range tailored to your individual needs and health conditions.
Hydration Considerations
Ensure proper hydration while managing sodium levels. Drink electrolyte-replenishing fluids, which contain sodium and other essential minerals. Sports drinks or oral rehydration solutions can be beneficial, especially after physical activity or in hot weather.
Regular Monitoring
Regularly check sodium levels through blood tests as directed by your healthcare provider. This helps identify trends and allows for timely adjustments in your diet or medication. Based on results, modify your sodium intake under medical guidance.
If taking diuretics like Lasix, discuss adjustments to sodium intake with your healthcare team to prevent excessive depletion. Collaborating with a registered dietitian can also help create a balanced meal plan supporting sodium levels while addressing overall nutritional needs.
Patient Education on Lasix and Sodium Balance
Lasix can lead to sodium depletion, which may affect your overall health. To manage this risk, consider the following recommendations:
- Monitor Sodium Intake: Aim to include moderate amounts of sodium in your diet. Foods like table salt, canned soups, and processed snacks can be high in sodium, but consult your healthcare provider for personalized advice.
- Stay Hydrated: Drinking enough water is crucial. Proper hydration helps maintain balanced sodium levels. However, discuss fluid intake with your doctor to align with your treatment goals.
- Regular Check-ups: Schedule regular blood tests to monitor sodium levels. Communicate any symptoms such as muscle cramps, dizziness, or fatigue, which could indicate low sodium levels.
- Discuss Medications: Inform your healthcare provider about all medications you are taking. Some drugs can enhance the diuretic effect of Lasix, leading to a greater risk of sodium depletion.
- Dietary Adjustments: Incorporate foods that are naturally high in potassium as well, since maintaining a balance between sodium and potassium is important. Bananas, oranges, and spinach are good options.
By following these guidelines, you can effectively manage your sodium levels while taking Lasix. Always reach out to your healthcare provider for guidance tailored to your specific situation.