Minocycline can be tied to ototoxic effects, leading to potential hearing issues. Users of this antibiotic should remain vigilant about their hearing health and consider discussing any symptoms with a healthcare professional. Symptoms like ringing in the ears or sudden hearing loss may not be immediately linked to medication usage, but they warrant immediate attention.
Research indicates that while ototoxicity related to minocycline is not the most common side effect, case reports do exist. These accounts highlight the risk of auditory damage, particularly with prolonged use or high doses. If you experience changes in hearing, consult your doctor promptly to evaluate the situation and discuss alternative treatments.
Being proactive about your health can make a difference. Keep track of any unusual auditory symptoms during your treatment with minocycline. Adopting preventive measures, such as regular hearing tests, can help catch potential issues early, allowing for timely intervention and care. Your hearing is important, and staying informed is the first step in safeguarding it.
- Understanding Minocycline Ototoxicity
- Risk Factors
- Preventive Measures
- Mechanisms of Ototoxicity Related to Minocycline
- Cellular Mechanisms
- Neurotransmitter Disruption
- Symptoms and Clinical Presentation of Minocycline-Induced Ototoxicity
- Risk Factors for Developing Ototoxicity from Minocycline
- Diagnosis and Assessment of Ototoxic Effects from Minocycline
- Management Strategies for Minocycline Ototoxicity
Understanding Minocycline Ototoxicity
Minocycline can lead to ototoxicity, particularly in individuals with pre-existing conditions or those taking high doses. Monitoring hearing function is crucial for patients prescribed this antibiotic, especially during prolonged treatment periods. If signs of hearing changes such as tinnitus or a decrease in hearing acuity occur, it is essential to consult a healthcare provider promptly.
Risk Factors
Several factors increase the likelihood of ototoxicity with minocycline. A history of hearing loss or current use of other ototoxic medications, such as certain diuretics or aminoglycosides, raises concern. Individuals with renal impairment should use minocycline cautiously due to altered drug clearance, enhancing the risk of side effects. Pregnant individuals or nursing mothers also should consider potential impacts on the developing fetus or infant.
Preventive Measures
To minimize the risk of ototoxicity, healthcare providers should establish thorough patient histories prior to prescribing minocycline. Regular audiometric evaluations may help catch any auditory changes early. Encourage patients to report any auditory symptoms and ensure they understand the importance of adherence to follow-up appointments. Education about potential risks empowers patients to take proactive steps in managing their health.
Mechanisms of Ototoxicity Related to Minocycline
Minocycline can induce ototoxicity through several mechanisms that impact auditory function. Understanding these pathways is key for healthcare providers and patients.
Cellular Mechanisms
Minocycline affects the inner ear cells, particularly hair cells, through the following actions:
- Apoptosis: Minocycline can trigger cell death in the cochlea, leading to a reduction in the number of functional hair cells.
- Inflammation: This antibiotic has been associated with inflammatory responses in the cochlea, which can disrupt normal auditory processing.
- Oxidative Stress: Minocycline may elevate oxidative stress levels, damaging cellular structures and impairing auditory cell function.
Neurotransmitter Disruption
Minocycline also influences neurotransmitter systems:
- Glutamate Modulation: This drug interferes with glutamate release, leading to excitotoxicity, particularly in the auditory pathways.
- Inhibition of Neurotransmitter Reuptake: Disruption in neurotransmitter balance can affect communication between auditory neurons and compromise hearing ability.
Regular monitoring for auditory symptoms in patients prescribed minocycline is advised. If signs of ototoxicity appear, consider alternative medications or consultations with an audiologist. Awareness and early intervention can help mitigate hearing loss associated with this antibiotic.
Symptoms and Clinical Presentation of Minocycline-Induced Ototoxicity
Recognizing the signs of minocycline-induced ototoxicity is crucial for timely intervention. Patients may report tinnitus, characterized by ringing or buzzing sounds in the ears, which can range in intensity. Auditory disturbances often manifest as hearing loss, typically affecting high frequencies initially. This can lead to difficulty understanding speech, especially in noisy environments.
Another common symptom includes vertigo, resulting in a sensation of spinning or dizziness. This can be disorienting and may impact daily activities. Additionally, patients might experience a feeling of fullness or pressure in the ears, which can be uncomfortable and concerning.
As symptoms progress, careful monitoring of auditory function becomes essential. In clinical evaluations, audiometric tests can reveal diminished hearing thresholds. These tests help in assessing the extent of ototoxicity and guiding further management.
Routine follow-ups with audiologists can facilitate early detection of changes in hearing. Patients experiencing these symptoms should consult their healthcare provider promptly to discuss the potential link with minocycline and explore alternatives, if necessary.
Awareness and education about these symptoms can enhance patient outcomes. Maintaining open communication about any auditory changes during treatment can significantly aid in addressing ototoxicity swiftly.
Risk Factors for Developing Ototoxicity from Minocycline
Several key factors contribute to the risk of developing ototoxicity from minocycline. Awareness of these can assist in monitoring and reducing potential harm.
Age plays a significant role; the elderly often display increased sensitivity to ototoxic effects due to age-related changes in the auditory system. Children may also be at risk, particularly when prescribed higher dosages.
Patients with pre-existing renal impairment face a heightened risk. Regular monitoring of kidney function is prudent for those receiving minocycline, as decreased renal clearance can exacerbate drug accumulation and toxicity.
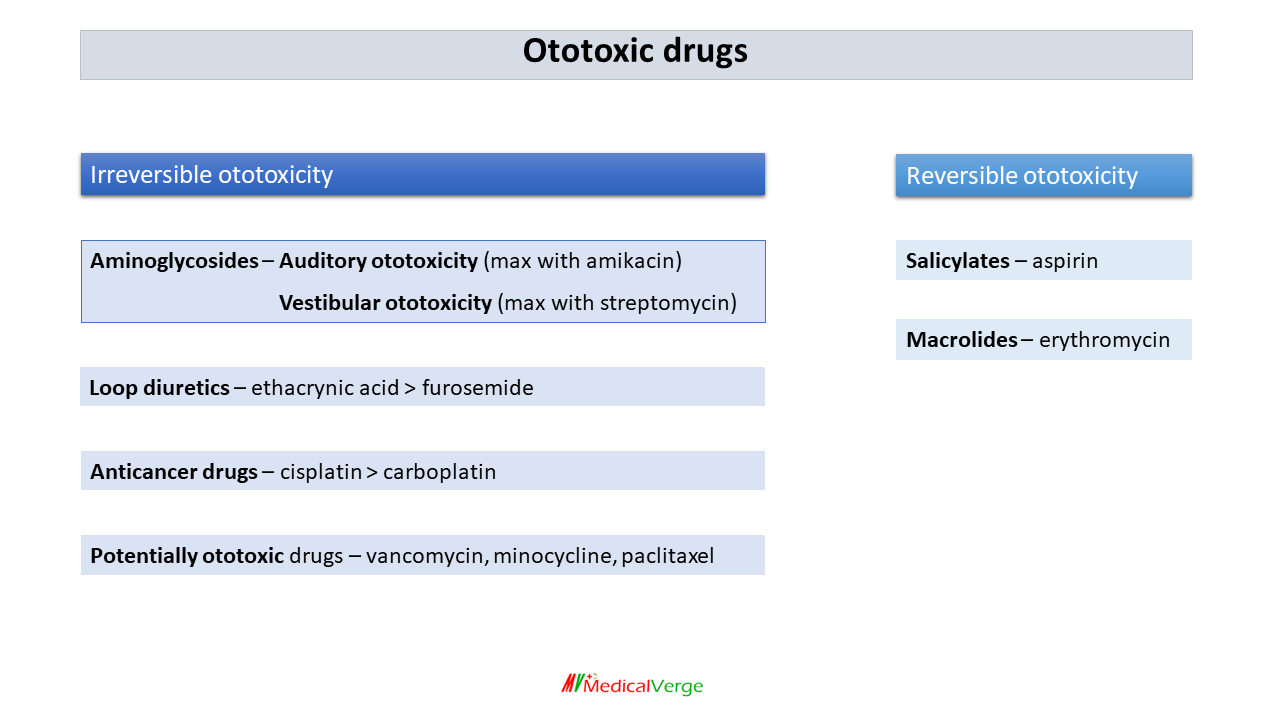
Concurrent use of other ototoxic agents, such as aminoglycosides or salicylates, increases the likelihood of hearing damage. A thorough medication review can help identify and mitigate this risk.
Duration of therapy is another crucial factor. Prolonged exposure to minocycline raises the chance of adverse auditory effects. Limiting treatment duration where possible, while maintaining adequate therapeutic response, is advisable.
Genetic predisposition also influences susceptibility. Patients with a family history of hearing loss or related conditions might require more vigilant monitoring during treatment.
| Risk Factor | Description |
|---|---|
| Age | Increased sensitivity in elderly and young patients. |
| Renal Impairment | Decreased clearance can lead to drug accumulation. |
| Concurrent Ototoxic Medications | Use with other ototoxic drugs heightens risk. |
| Duration of Treatment | Longer exposure can increase aural toxicity. |
| Genetic Factors | Family history of hearing loss raises susceptibility. |
Awareness and monitoring of these risk factors can help mitigate the potential for ototoxicity during minocycline treatment. Regular audiometric assessments provide a proactive approach to managing hearing health in at-risk individuals.
Diagnosis and Assessment of Ototoxic Effects from Minocycline
Monitor patients receiving minocycline for signs of ototoxicity, including tinnitus, hearing loss, or balance disturbances. A thorough patient history focusing on pre-existing auditory conditions is crucial. Document any concurrent ototoxic medications or high-risk factors, such as a history of renal impairment.
Conduct a baseline audiological evaluation prior to starting minocycline. Regular hearing assessments during treatment can help catch early signs of ototoxic effects. Pure-tone audiometry and speech discrimination scores provide valuable insights into auditory function.
If ototoxicity is suspected, promptly consult an audiologist for a detailed evaluation. Consider discontinuing minocycline or adjusting the dosage if confirmed ototoxic effects are present. Supportive care may include referral to an ear, nose, and throat specialist for further assessment and potential management options.
Educate patients about recognizing symptoms of ototoxicity and encourage them to report any changes in hearing or balance immediately. This proactive approach aids in timely diagnosis and intervention, minimizing the long-term impact on auditory health.
Management Strategies for Minocycline Ototoxicity
Monitor hearing function regularly in patients receiving minocycline. Audiometric assessments help detect early signs of ototoxicity, allowing for prompt interventions.
Adjust the dosage of minocycline based on renal function. Reduction in dosage can mitigate risks associated with ototoxicity, particularly in patients with pre-existing kidney conditions.
Educate patients about potential auditory symptoms such as tinnitus or hearing changes. Encourage them to report any unusual symptoms immediately for timely evaluation.
Consider alternative antibiotics when appropriate. Evaluate the necessity of minocycline for treatment and assess other treatment options that carry a lower risk of ototoxicity.
Involve an audiologist for further evaluation and management of hearing-related issues. Audiologists can provide specialized assessments and recommend rehabilitation options if hearing loss occurs.
Implement interdisciplinary care involving physicians, audiologists, and pharmacists. This team approach ensures comprehensive management and monitoring of patients on minocycline.
Utilize patient education materials that outline the risks of ototoxicity with minocycline. Increase awareness and encourage adherence to follow-up appointments for auditory assessments.
Document any reported cases of ototoxicity in the patient’s medical records. This information aids in tracking trends and improving future patient management strategies.
Support usage of hearing conservation strategies if ototoxicity is suspected. Provide resources for counseling and auditory training to enhance coping mechanisms for affected patients.