Nimotop, containing the active ingredient nimodipine, stands out for its targeted action on cerebral blood vessels. This medication is primarily used to prevent neurological deficits following subarachnoid hemorrhage due to aneurysmal rupture. Administering Nimotop within 96 hours of the incident can significantly enhance blood flow to the brain, reducing the risk of complications.
For optimal results, clinicians recommend a specific dosage tailored to the patient’s condition. Generally, the starting dose for adults is 30 mg every four hours. This regimen should be maintained for a duration of two weeks, allowing for gradual improvement in cerebral perfusion. Patients must not take more than the prescribed amount as this can lead to side effects, including hypotension or tachycardia.
Regular monitoring of blood pressure during treatment is advisable to ensure patient safety. If adverse reactions occur, consulting a healthcare professional promptly is essential. Nimotop may also interact with certain medications, so a thorough review of a patient’s current prescriptions is critical prior to initiating therapy.
- Nimotop Medication: A Comprehensive Overview
- Indications and Uses
- Dosing and Administration
- What is Nimotop Medication?
- Indications and Uses of Nimotop
- Specific Uses
- Administration Guidelines
- Mechanism of Action of Nimotop
- Key Effects
- Clinical Implications
- Dosage and Administration Guidelines for Nimotop
- Adjustments for Specific Populations
- Monitoring and Duration of Treatment
- Potential Side Effects and Adverse Reactions
- Drug Interactions with Nimotop
- Contraindications and Precautions for Nimotop Use
- Patient Monitoring and Follow-Up Care on Nimotop
- Key Parameters to Monitor
- Follow-Up Schedule
Nimotop Medication: A Comprehensive Overview
Nimotop, containing the active ingredient nimodipine, serves as a calcium channel blocker with specific efficacy in neurology. It primarily aids in improving cerebral blood flow, particularly following subarachnoid hemorrhage. Clinicians often recommend it post-hemorrhage to mitigate complications like vasospasm, enhancing recovery outcomes.
Indications and Uses
This medication specifically targets neurological conditions, especially those linked to impaired blood circulation in the brain. Physicians prescribe Nimotop to enhance recovery from ischemic events, particularly after a stroke or brain injury. Its ability to selectively dilate cerebral blood vessels highlights its significance in managing brain health.
Dosing and Administration
Nimotop is typically administered orally, with a standard dose of 30 mg every 4 hours for 21 consecutive days. Consistency is key; adhering to the schedule optimizes therapeutic benefits. Swallow the capsules whole, avoiding crushing or chewing. For patients unable to take medications orally, intravenous options may be considered under strict medical supervision.
Monitoring is crucial during treatment. Regular assessments of blood pressure and heart rate help ensure safety, as Nimotop can cause hypotension. Adjusting the dose may be necessary based on individual patient response and specific health conditions.
Consult healthcare professionals before starting Nimotop, especially for those with allergies, liver issues, or concurrent use of other medications. Understanding potential drug interactions and side effects promotes safer use.
The therapeutic role of Nimotop extends beyond mere symptom management; it actively contributes to improved neurological outcomes. Incorporating this medication into a broader treatment strategy can significantly influence recovery trajectories in affected patients.
What is Nimotop Medication?
Nimotop, containing the active ingredient nimodipine, primarily treats subarachnoid hemorrhage from aneurysmal rupture. It works by relaxing blood vessels, improving blood flow to the brain, and reducing the risk of brain damage due to lack of oxygen.
This medication is administered orally, typically in tablet form or as a solution, with the goal of maintaining optimal blood circulation after a brain bleed. Adhering to the prescribed dosage is crucial for its efficacy and minimizing potential side effects.
Common side effects may include headaches, dizziness, and gastrointestinal disturbances. Monitoring by healthcare providers is essential to ensure safety, especially for individuals with pre-existing heart conditions.
Here’s a quick overview of the key features of Nimotop:
| Characteristic | Description |
|---|---|
| Active Ingredient | Nimodipine |
| Indication | Subarachnoid hemorrhage |
| Administration | Oral tablets or solution |
| Common Side Effects | Headaches, dizziness, gastrointestinal issues |
| Monitoring | Required for individuals with heart conditions |
Consult a healthcare professional for personalized advice, especially regarding interactions with other medications. Staying informed is the best approach to using Nimotop effectively and safely.
Indications and Uses of Nimotop
Nimotop is primarily used for the prevention of neurological deficits following a subarachnoid hemorrhage (SAH). This medication helps improve cerebral blood flow, reducing the risk of complications associated with SAH, such as ischemic deficits. Healthcare providers often recommend it in acute settings to enhance recovery prospects.
Specific Uses
- Subarachnoid Hemorrhage: Nimotop is indicated when patients experience SAH to mitigate neurological damage.
- Cerebral Vasospasm: It assists in preventing vasospasm, a common complication post-SAH.
- Improving Cognitive Outcomes: Some studies suggest it may aid in cognitive recovery during rehabilitation.
Administration Guidelines
- Administer as soon as possible after SAH onset.
- Follow dosing instructions provided by health professionals to ensure optimal outcomes.
- Monitor patients for potential side effects, particularly if they have existing cardiovascular conditions.
Always consult a healthcare professional for personalized advice and to understand the best use of Nimotop in individual cases.
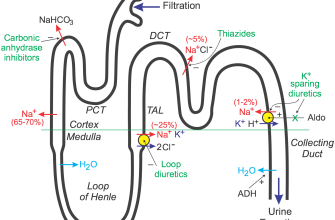
Mechanism of Action of Nimotop
Nimotop primarily functions as a calcium channel blocker, specifically targeting L-type calcium channels. By inhibiting these channels, it effectively reduces the influx of calcium ions into vascular smooth muscle and myocardial cells. This action leads to vasodilation, which decreases vascular resistance and enhances blood flow, particularly in the brain.
Key Effects
- Reduces calcium ion entry, promoting relaxation of smooth muscles.
- Improves cerebral blood flow, aiding recovery from ischemia.
- Enhances oxygen supply to the brain, minimizing damage in stroke patients.
Additionally, Nimotop has neuroprotective properties. It helps stabilize cellular membranes and inhibits excitotoxicity caused by excessive neurotransmitters. This contributes to neuronal preservation during conditions like subarachnoid hemorrhage.
Clinical Implications
- Administered in cases of acute subarachnoid hemorrhage to prevent complications.
- Utilized in patients with vasospasm to maintain cerebral perfusion.
By improving cerebral blood flow and providing neuroprotection, Nimotop plays a significant role in treating specific neurological conditions, making it a valuable medication in therapeutic settings. Regular monitoring and dosage adjustments ensure optimal results for patients.
Dosage and Administration Guidelines for Nimotop
The usual starting dosage for Nimotop is 30 mg every 4 hours, totaling six doses per day. Administer the medication orally for maximum absorption. Ensure that doses are evenly spaced throughout the day to maintain consistent therapeutic levels in the bloodstream.
For patients unable to take oral medication due to specific conditions, consider administering Nimotop via intravenous infusion. The typical intravenous dosage is 0.5 mg/hour. Monitor the patient’s response closely while adjusting the dose as necessary based on their clinical condition and tolerability.
Adjustments for Specific Populations
Older adults may require a reduced dosage due to potential changes in drug metabolism. Initiate therapy at a lower dose, observing the patient’s response before increasing. Patients with liver dysfunction might also need dosage adjustments. Conduct regular liver function tests to guide treatment modifications.
Monitoring and Duration of Treatment
Monitor blood pressure, heart rate, and overall patient condition regularly during treatment with Nimotop. The duration of therapy generally lasts for several weeks, based on the individual response and condition being treated. Evaluate the treatment progress at regular intervals to determine the necessity of continued use.
Potential Side Effects and Adverse Reactions
Nimotop may cause several side effects, which can vary in severity. Monitoring your health during treatment is important, as this enables timely identification of any adverse reactions.
- Headaches: Some patients report headaches, which can be managed with typical pain relief medications.
- Dizziness: Dizziness may occur, particularly when standing up quickly. Staying hydrated and moving slowly can help mitigate this effect.
- Nausea: Nausea can be experienced by some individuals. Taking Nimotop with food might reduce the likelihood of this side effect.
- Pupil dilation: Some people may notice changes in pupil size. This effect is generally temporary.
In rare cases, more severe side effects can arise. Seek medical attention if you experience:
- Severe allergic reactions: Symptoms may include rash, itching, swelling, or difficulty breathing.
- Chest pain: This might indicate a serious condition requiring immediate evaluation.
- Heart palpitations: Unusual heartbeat patterns should be discussed with a healthcare provider.
Always consult your healthcare professional if any side effects persist or worsen. Individual responses to medication differ, so staying informed will help ensure safety during treatment with Nimotop.
Drug Interactions with Nimotop
Nimotop may interact with several medications, influencing their effects. Always consult a healthcare provider before combining it with other treatments. Common interactions include the use of antihypertensives, which may enhance the blood pressure-lowering effects of Nimotop, leading to hypotension. Monitor blood pressure regularly when these medications are taken together.
Additionally, concomitant use with other calcium channel blockers can increase the risk of side effects. Adjustments in dosage or careful monitoring may be necessary in such cases. Patients on antiarrhythmic drugs should also be cautious, as these medications can interact with Nimotop, affecting heart rhythm.
Antibiotics like erythromycin or antifungals such as ketoconazole might alter the metabolism of Nimotop, potentially increasing its concentration in the blood. This can raise the risk of adverse effects. Regular monitoring is advisable if these medications are prescribed concurrently.
Avoid alcohol consumption while taking Nimotop. Alcohol can exacerbate side effects like dizziness and drowsiness. Disclose all medications, including over-the-counter drugs and supplements, to your healthcare provider to ensure safe use together.
Routine follow-up appointments are crucial for adjusting therapies as needed. Keeping an open dialogue with your healthcare team helps manage any potential interactions effectively.
Contraindications and Precautions for Nimotop Use
Nimotop is contraindicated in individuals with hypersensitivity to nimodipine or any of its components. Patients with severe hypotension or circulatory shock should avoid using this medication, as it may exacerbate these conditions.
Consider avoiding Nimotop in cases of coronary artery disease, as it can lead to myocardial ischemia due to its vasodilatory effects. Caution is necessary when prescribing Nimotop to patients with hepatic impairment, as it can alter drug metabolism and increase the risk of side effects.
| Condition | Recommendation |
|---|---|
| Hypersensitivity | Do not use. |
| Severe hypotension | Avoid use. |
| Coronary artery disease | Use with caution. |
| Hepatic impairment | Adjust dosage. |
Regular monitoring of blood pressure is advised, especially during the initial treatment phase. Advise patients to report any signs of dizziness, lightheadedness, or unusual heartbeats. Discuss potential interactions with other medications, particularly those affecting blood pressure, to prevent adverse events.
Pediatric use has not been adequately studied; therefore, exercise caution when considering Nimotop for children. Pregnancy Category C indicates that its safety has not been established, so weigh the benefits against risks before prescribing during pregnancy or breastfeeding.
Patient Monitoring and Follow-Up Care on Nimotop
Regular monitoring of patients on Nimotop is crucial. Schedule initial assessments within the first week of treatment. Conduct neurological examinations to evaluate cognitive function and assess any side effects.
Key Parameters to Monitor
Pay attention to blood pressure, heart rate, and any signs of hypotension, as these can occur with Nimotop use. Track changes in symptoms and document any adverse reactions. Encourage patients to report headaches, dizziness, or gastrointestinal issues immediately.
Follow-Up Schedule
Plan follow-up visits every 4 to 6 weeks during the first three months. After stabilization, extend the intervals based on the patient’s progress. Use these sessions to reinforce treatment compliance and address any concerns. Regular blood tests may be necessary to assess liver function and electrolyte levels.
Educate patients about the importance of adhering to the prescribed dosage. Remind them to avoid sudden discontinuation of the medication, as this may lead to rebound symptoms.
In cases of new or worsening symptoms, reassess the treatment plan promptly. Collaborate with other healthcare providers to ensure a multidisciplinary approach to patient care.