Monitor for signs of bleeding while taking prednisone, as this medication may increase the risk. Patients using prednisone should be vigilant about any unusual bruising, prolonged bleeding from cuts, or blood in urine and stool. Early detection can prevent complications and ensure timely medical intervention.
Consult with your healthcare provider if you notice any of these symptoms. They may recommend adjustments in dosage or additional medications to manage bleeding risks effectively. It’s also wise to discuss the use of other drugs, such as non-steroidal anti-inflammatory drugs (NSAIDs), which can exacerbate bleeding when taken alongside prednisone.
Regular follow-ups are essential. Routine blood tests can help gauge your platelet levels and monitor for any changes that might indicate increased bleeding risk. Adhering to these practices not only enhances your safety but also contributes to a smoother treatment experience.
- Prednisone and Bleeding: A Detailed Overview
- Risk Factors for Bleeding
- Precautionary Measures
- Understanding Prednisone: Uses and Mechanism
- Mechanism of Action
- Usage Considerations
- Common Side Effects of Prednisone Related to Bleeding
- Gastrointestinal Issues
- Impact on Blood Clotting
- Risk Factors for Bleeding While on Prednisone
- Symptoms Indicating Potential Bleeding Issues
- GI Symptoms
- Oral and Nasal Symptoms
- Managing Bleeding Risks During Prednisone Therapy
- Dietary Considerations
- Monitoring and Symptoms
- When to Seek Medical Attention for Bleeding Concerns
- Signs of Serious Bleeding
- Factors to Consider
- Alternatives to Prednisone for Patients with Bleeding Risks
- Corticosteroid Alternatives
- Immunosuppressants
Prednisone and Bleeding: A Detailed Overview
Patients taking prednisone should monitor for any signs of bleeding. This medication can affect blood clotting and may increase the risk of gastrointestinal bleeding. Short-term use generally poses a lower risk, but prolonged treatment can lead to more significant complications.
Risk Factors for Bleeding
Several factors heighten the bleeding risk during prednisone therapy. Co-administration of non-steroidal anti-inflammatory drugs (NSAIDs) increases the likelihood of gastrointestinal issues. Individuals with a history of ulcers or gastrointestinal disorders face greater hazards. Additionally, those with bleeding disorders or those on anticoagulant medications must exercise caution.
Precautionary Measures
Regular check-ups are essential for patients on prednisone. Discuss any medications you take with your healthcare provider to assess potential interactions. If any signs of bleeding–such as tarry stools, unusual bruising, or prolonged bleeding from cuts–occur, seek medical attention immediately. Using proton pump inhibitors can protect the stomach lining and minimize bleeding risk when taking prednisone concurrently with NSAIDs.
Understanding Prednisone: Uses and Mechanism
Prednisone is commonly prescribed to reduce inflammation and suppress the immune system. It proves beneficial in treating conditions such as asthma, rheumatoid arthritis, and certain autoimmune diseases. Healthcare providers frequently recommend it for short-term management of acute flare-ups as well as for long-term treatment of chronic conditions.
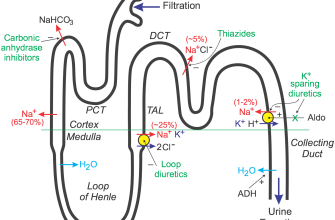
Mechanism of Action
Prednisone functions through its conversion to prednisolone in the liver, where it then interacts with glucocorticoid receptors in cells. This interaction leads to the modulation of gene expression and reduces the production of inflammatory mediators. As a result, it diminishes swelling, redness, and pain associated with inflammatory processes. Additionally, it suppresses T-lymphocyte activation, which plays a significant role in the immune response.
Usage Considerations
While effective, prednisone can cause side effects, including weight gain, mood changes, and increased blood sugar levels. It’s critical to monitor these effects regularly. Adjustments to dosage and duration of therapy may be necessary, and healthcare providers might suggest lifestyle modifications to counteract certain side effects. Always consult a healthcare professional before making any changes to your medication regimen.
Common Side Effects of Prednisone Related to Bleeding
Prednisone can lead to specific side effects that increase the risk of bleeding, particularly when used for extended periods or at high doses. Patients taking this medication should be vigilant about changes in their bodies that could indicate bleeding complications.
Gastrointestinal Issues
The most notable risk involves gastrointestinal problems. Prolonged use of prednisone may cause gastric irritation and ulcers. This irritation can lead to symptoms like stomach pain, nausea, or black stools, indicating potential bleeding. To mitigate these risks, consider taking prednisone with food, and consult a healthcare provider about using stomach-protecting medications such as proton pump inhibitors (PPIs) or antacids.
Impact on Blood Clotting
Prednisone affects blood clotting by altering platelet function. Thinning of the blood can occur, increasing susceptibility to bruising and spontaneous bleeding. Monitor for easy bruising or unusual bleeding from minor cuts or scrapes. If bleeding is excessive or persistent, contact a healthcare professional promptly.
Risk Factors for Bleeding While on Prednisone
Taking prednisone increases the risk of bleeding, especially in individuals with certain conditions. One significant factor is the presence of underlying health issues such as liver disease, which can impair blood clotting. Patients with gastrointestinal disorders, including peptic ulcers or inflammatory bowel disease, also face heightened bleeding risks.
Concurrent use of non-steroidal anti-inflammatory drugs (NSAIDs) can exacerbate the potential for bleeding. Combining prednisone with medications that affect platelet function or anticoagulants raises the likelihood of hemorrhagic complications. It’s crucial to inform healthcare providers of all medications being taken to assess the risk effectively.
Age contributes to increased vulnerability. Older adults often have multiple health concerns, including frailer blood vessels and slower healing processes, making them more susceptible to bleeding. Similarly, high-dose prednisone therapy amplifies the risk due to its greater impact on the body’s ability to manage inflammation and clotting.
Underlying conditions, such as diabetes, can also complicate the situation. Diabetes may affect circulation and wound healing, which can lead to an increased risk of bleeding. Regular monitoring and timely interventions are essential for patients with such risk factors.
Prior history of bleeding events should prompt careful monitoring for anyone starting prednisone therapy. This includes evaluating family history, as genetic predispositions might play a role. By understanding these risk factors, patients and healthcare providers can implement strategies to mitigate bleeding risks while managing the primary condition effectively.
Symptoms Indicating Potential Bleeding Issues
Watch for unusual bruising, especially if it appears without any apparent cause. Frequent or unusually large bruises can indicate a bleeding disorder. If you notice red or purple spots on your skin, known as petechiae, take it as a signal to consult a healthcare provider.
GI Symptoms
Pay attention to any changes in your bowel movements. Dark, tarry stools may signal internal bleeding, typically from the upper gastrointestinal tract. Bright red blood in stool can indicate bleeding from the lower gastrointestinal tract. Both require immediate medical evaluation.
Oral and Nasal Symptoms
Frequent nosebleeds or bleeding gums can be red flags. If you experience these symptoms regularly, particularly when brushing your teeth, seek a professional opinion. Persistent or excessive bleeding from minor cuts or scrapes also warrants further investigation.
If you encounter fatigue, weakness, or dizziness, especially in conjunction with any of the above symptoms, reach out to a healthcare provider. These signs may suggest anemia due to blood loss. Regular monitoring and prompt action can help address potential bleeding issues effectively.
Managing Bleeding Risks During Prednisone Therapy
Monitor your liver function tests regularly. Prednisone can affect liver enzymes, increasing the risk of bleeding. If abnormalities appear, consult your healthcare provider.
Communicate with your doctor about any existing conditions. Conditions such as liver disorder, kidney disease, or coagulopathy may heighten bleeding risks while on prednisone.
Be aware of interactions with other medications. Non-steroidal anti-inflammatory drugs (NSAIDs), anticoagulants, or certain antibiotics can amplify bleeding risks. Maintain a current medication list to discuss with your physician.
Dietary Considerations
- Include foods rich in vitamin K. Leafy greens can help support blood clotting.
- Avoid excessive alcohol intake. Alcohol can elevate the risk of gastrointestinal bleeding while on prednisone.
Monitoring and Symptoms
Conduct regular self-checks for any signs of bleeding. Common symptoms include:
- Unusual bruising
- Blood in urine or stools
- Prolonged bleeding from cuts
If you experience these symptoms, seek medical attention immediately. Early intervention can prevent serious complications.
Maintain open dialogue with your healthcare provider throughout therapy. Regular reviews of your treatment plan can adjust dosages or explore alternatives if bleeding risks become concerning.
When to Seek Medical Attention for Bleeding Concerns
If you notice any unusual or excessive bleeding, consult a healthcare provider immediately. Pay close attention to the following signs that indicate the need for urgent medical care:
Signs of Serious Bleeding
- Bright red blood in stool or urine
- Vomiting blood or coffee-ground-like material
- Severe cuts or injuries that won’t stop bleeding
- Menstrual bleeding that soaks through a pad or tampon every hour for several hours
- Signs of internal bleeding, such as sudden and severe pain, fainting, or confusion
Factors to Consider
Assess your situation by considering these factors:
- Your use of prednisone or other anticoagulants, as these can increase bleeding risks
- Any underlying health conditions, such as liver disease or hemophilia
- Recent surgeries or procedures that may contribute to bleeding
- Continuous bleeding lasting more than 10 minutes
Being proactive about these signs and factors can help ensure your safety and well-being. Don’t hesitate to reach out to a medical professional if you have doubts about your symptoms.
Alternatives to Prednisone for Patients with Bleeding Risks
Consider using other anti-inflammatory medications that pose a lower risk of bleeding complications. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen generally carry a risk of gastrointestinal bleeding, so they may not be ideal for these patients. Instead, medications like celecoxib, a selective COX-2 inhibitor, can offer pain relief with a reduced bleeding risk.
Corticosteroid Alternatives
Topical corticosteroids like hydrocortisone or triamcinolone can be effective for localized conditions without systemic side effects. Inhaled corticosteroids also provide anti-inflammatory benefits for respiratory issues while minimizing risks associated with oral prednisone.
Immunosuppressants
Azathioprine and methotrexate are alternatives for managing autoimmune disorders. They work to suppress the immune response without the heightened bleeding risks associated with corticosteroids. Monitor patients closely for liver function and blood counts while on these medications.
| Medication | Type | Bleeding Risk |
|---|---|---|
| Celecoxib | COX-2 Inhibitor | Lower |
| Hydrocortisone | Topical Corticosteroid | Very Low |
| Aza-thioprine | Immunosuppressant | Moderate |
| Methotrexate | Immunosuppressant | Moderate |
Always consult with healthcare providers to determine the most suitable option based on individual patient profiles, including specific medical histories and current medications. Regular monitoring enhances safety and efficacy for those at risk of bleeding.