The biological half-life of prednisone is approximately 3 to 4 hours in healthy individuals. This timeframe indicates how long it takes for half of the drug to be eliminated from the body, which is crucial for determining dosing schedules. Understanding this half-life assists healthcare providers in tailoring the therapy according to the specific needs of patients.
For patients on long-term prednisone therapy, maintaining stable drug levels in the bloodstream is essential. Typically, dosing is adjusted based on the indication for use, and many practitioners recommend administering doses once daily in the morning to align with the body’s natural cortisol rhythm. This approach minimizes potential side effects and enhances therapeutic efficacy.
Factors such as age, liver function, and concurrent medications can influence the metabolism of prednisone. For instance, older adults may experience prolonged half-life due to decreased hepatic function. Monitoring these factors allows for personalized management of prednisone treatment, ensuring optimal outcomes.
Ultimately, understanding the biological half-life of prednisone supports informed decision-making in treatment. Effective management leads to better control of conditions such as autoimmune disorders or inflammation while minimizing the risks associated with prolonged use.
- Biological Half-Life of Prednisone
- Factors Influencing Half-Life
- Dosing Considerations
- Understanding Prednisone: A Brief Overview
- Dosage and Administration
- Biological Half-Life
- What is Biological Half-Life?
- Factors Influencing the Biological Half-Life of Prednisone
- Comparative Half-Life: Prednisone vs. Other Corticosteroids
- Methylprednisolone
- Dexamethasone
- Clinical Implications of Prednisone’s Half-Life
- Measuring the Half-Life of Prednisone in Clinical Practice
- Blood Sampling Protocols
- Interpreting Results
- Adjusting Dosage Based on Half-Life: A Practical Guide
- Future Research Directions on Prednisone Metabolism
- Exploration of Drug-Drug Interactions
- Role of Gut Microbiome
Biological Half-Life of Prednisone
The biological half-life of prednisone ranges from 3 to 4 hours, although this can vary based on individual factors like metabolism, dosage, and the presence of other medical conditions. It’s crucial to consider that this half-life is influenced by how the body processes and eliminates the medication.
Factors Influencing Half-Life
Several factors can affect the half-life of prednisone, including:
- Age: Older adults may metabolize prednisone more slowly, leading to a longer half-life.
- Kidney Function: Impaired kidney function can extend the half-life due to reduced clearance of the drug.
- Liver Function: Prednisone is metabolized in the liver, so any hepatic insufficiency can prolong its half-life.
- Dosage: Higher doses might lead to accumulation, affecting the effective half-life.
Dosing Considerations
When planning dosing schedules, consider the half-life alongside the therapeutic effects. For conditions requiring consistent steroid levels, a more frequent dosing might be necessary. A careful balance will help maintain effective drug levels in the bloodstream while minimizing side effects.
| Condition | Dosing Recommendation |
|---|---|
| Severe Inflammation | Initial doses may be higher, tapering as symptoms improve. |
| Chronic Conditions | Lower doses may be required for maintenance therapy. |
| Aspiration Disorders | Consider alternate-day dosing to reduce side effects. |
Adjustments to dosing should always be made under medical supervision to ensure safety and efficacy.
Understanding Prednisone: A Brief Overview
Prednisone serves as a synthetic corticosteroid effective in reducing inflammation and suppressing the immune response. It’s commonly prescribed for conditions like asthma, rheumatoid arthritis, and certain autoimmune disorders.
Dosage and Administration
When taking prednisone, follow your healthcare provider’s recommendations for dosage. Adjustments may occur based on your specific condition and response to treatment. Taking it with food can help minimize gastrointestinal discomfort. Avoid abrupt discontinuation without medical advice, as tapering is generally necessary to prevent withdrawal symptoms.
Biological Half-Life
The biological half-life of prednisone varies, typically ranging from 3 to 4 hours in healthy individuals. This duration can extend if the drug is used frequently or at higher dosages. Understanding this half-life is crucial for optimizing therapeutic effects while minimizing side effects.
Monitoring blood levels might be appropriate in certain cases to ensure consistent drug levels. Stay vigilant for signs of potential side effects, such as increased appetite, mood changes, or changes in blood sugar levels.
Prednisone can interact with other medications, so provide a complete list of current medications to your healthcare provider. Regular follow-ups ensure that your treatment remains effective and safe.
What is Biological Half-Life?
Biological half-life refers to the time required for the concentration of a substance, such as a drug, to reduce to half of its initial amount in the body. Understanding biological half-life helps in determining dosing schedules and predicting drug interactions.
This measurement is crucial for evaluating how long a medication remains effective and when it needs to be administered again. For prednisone, a synthetic corticosteroid, the half-life can influence treatment outcomes, patient adherence, and the management of potential side effects.
Several factors affect the biological half-life of a drug:
- Metabolism: The liver processes drugs into inactive or active metabolites. An increase in metabolic rate can shorten half-life.
- Age: Older adults may have altered metabolism and excretion rates, potentially prolonging half-life.
- Health conditions: Impairments in liver or kidney function can lead to an increased half-life as drugs are eliminated less effectively.
- Body composition: Fat and water distribution can also affect how long a drug remains in circulation.
For precise dosing and effective therapy, it is advisable to monitor specific pharmacokinetic parameters, including the biological half-life, in patients receiving prednisone or other medications. Adjustments to the dosage may be necessary based on these individual characteristics to optimize treatment outcomes.
Factors Influencing the Biological Half-Life of Prednisone
Various factors can impact the biological half-life of prednisone. Individual metabolism plays a significant role. People with faster metabolic rates may process the drug more quickly, leading to a shorter half-life. In contrast, those with slower metabolisms might experience prolonged effects due to slower clearance.
Aging affects drug metabolism as well. Older adults often exhibit reduced liver function and altered kidney capacity, which can increase the half-life of prednisone. This change necessitates careful dosage adjustments for elderly patients to avoid potential complications.
Another factor is body weight. Higher body mass can influence the distribution and clearance of prednisone. Individuals with increased fat mass may retain the drug longer, affecting its overall activity and duration in the system.
Liver health is critical. Conditions such as cirrhosis or hepatitis can impair drug metabolism, leading to an increased half-life for predisone. Monitoring liver function is essential during long-term treatment to avoid toxicity.
Drug interactions also play a key role. Concomitant use of medications that inhibit or induce liver enzymes can alter prednisone’s metabolism. Always consult healthcare providers about potential interactions, especially when starting or stopping other treatments.
Lastly, genetic factors can determine how individuals metabolize medications. Variations in specific genes responsible for drug metabolism can lead to differences in how long prednisone remains effective in the body. Genetic testing might be beneficial for determining optimal dosing strategies for some patients.
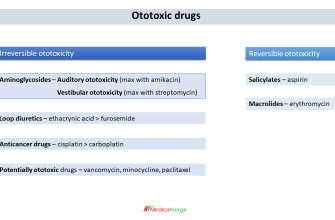
Comparative Half-Life: Prednisone vs. Other Corticosteroids
Prednisone has a biological half-life of approximately 3 to 4 hours, which differentiates it from other corticosteroids. Its rapid metabolism allows for quick adjustment of dosage in response to the patient’s needs. This characteristic is beneficial in managing acute conditions but may require more frequent dosing compared to longer-lasting alternatives.
Methylprednisolone
Methylprednisolone features a longer half-life, averaging about 18 to 36 hours. This extended duration enables once-daily dosing in many cases, which enhances patient compliance, especially for chronic conditions requiring consistent treatment. Its pharmacokinetics support prolonged anti-inflammatory effects.
Dexamethasone
Dexamethasone stands out with a half-life of up to 36 to 72 hours. This corticosteroid provides substantial anti-inflammatory effects and is often preferred in scenarios needing sustained control over inflammation. Its extended half-life minimizes the frequency of administration, making it suitable for severe cases where long-term therapy is necessary.
In choosing between these medications, consider the duration of action needed. Prednisone suits those requiring swift symptom relief, while methylprednisolone and dexamethasone cater to patients needing longer therapeutic effects with less frequent dosing. Each corticosteroid has unique properties that can influence treatment outcomes based on individual patient requirements.
Clinical Implications of Prednisone’s Half-Life
For optimal management of conditions treated with prednisone, it’s important to consider its biological half-life of approximately 3 to 4 hours. Tailoring dosing schedules around this time frame can enhance therapeutic outcomes and minimize side effects.
- Dosing Frequency: Administer prednisone multiple times throughout the day to maintain stable plasma levels. This approach reduces the risk of symptoms returning between doses.
- Time of Day: Consider morning dosing to align with the body’s natural cortisol production. This may improve patient tolerance and reduce potential insomnia.
- Monitoring Side Effects: Be vigilant for signs of adrenal suppression, especially in patients on long-term therapy. Regular evaluation helps manage risks associated with prolonged use.
- Adjustment for Specific Populations: Adjust dosing strategies for patients with renal or hepatic impairment as these conditions can affect prednisone metabolism and clearance.
- Comparison with Other Corticosteroids: Recognize that shorter half-lives of alternative corticosteroids may require different dosing strategies, affecting overall management plans.
Understanding prednisone’s pharmacokinetics guides clinicians in making informed decisions that enhance patient outcomes. Regularly revisit treatment plans and adjust based on patient response and side effect profiles.
Measuring the Half-Life of Prednisone in Clinical Practice
To accurately measure the half-life of prednisone in clinical settings, healthcare professionals should conduct a pharmacokinetic analysis that includes blood sampling at specified intervals. Typically, the half-life ranges from 2 to 4 hours in healthy individuals, but variations exist based on factors like dosage, metabolic rate, and patient health status.
Blood Sampling Protocols
For effective measurement, schedule blood draws at key points, specifically before and after administration. Collect samples at intervals of 30 minutes, 1 hour, 2 hours, and 4 hours post-dose. This timeframe allows for a more precise calculation of the drug’s elimination rate from the plasma.
Interpreting Results
Calculate the half-life using the following formula: Half-life = (0.693 × Volume of distribution) / Clearance. Adjust calculations based on individual patient factors, such as renal function and concurrent medications, as these can alter clearance rates. Monitoring the patient’s response to therapy will also guide dosage adjustments and overall treatment efficacy.
Adjusting Dosage Based on Half-Life: A Practical Guide
To optimize the therapeutic effects of prednisone, adjust the dosage based on its biological half-life of approximately 3 to 4 hours. Monitor the patient’s response closely and consider administering the medication two to four times daily to maintain stable blood levels.
When a patient experiences adverse effects or insufficient relief, reassess the dosage. Tapering the dose may be necessary for patients transitioning from higher doses or those encountering side effects. Gradually reducing the medication can help mitigate withdrawal symptoms and allow for better tolerance.
For patients with specific conditions, like autoimmune disorders, consider increasing the dosage during flare-ups and decreasing it during remission. This approach takes advantage of prednisone’s half-life, ensuring adequate control of symptoms while minimizing long-term side effects.
Assess renal and hepatic function before making adjustments. Impaired function may prolong the drug’s half-life, necessitating a lower dosage to avoid toxicity. Use clinical judgment and available lab results to tailor the treatment plan.
Encourage patients to report any changes in symptoms or side effects. Regular follow-ups allow for timely dose adjustments, ensuring the therapy remains as effective and safe as possible. Communication fosters a collaborative approach, leading to better outcomes.
In summary, effective management of prednisone therapy hinges on understanding its half-life. Employ a flexible dosing strategy, continuously monitor patient responses, and adjust appropriately to enhance therapeutic benefits while minimizing risks.
Future Research Directions on Prednisone Metabolism
Investigate the genetic factors influencing prednisone metabolism. Research indicates that polymorphisms in genes such as CYP3A4 and CYP3A5 significantly affect drug clearance and efficacy. Personalized medicine approaches could optimize dosing strategies based on an individual’s genetic makeup.
Exploration of Drug-Drug Interactions
Examine potential interactions with commonly prescribed medications. Understanding these interactions may enhance therapeutic outcomes and reduce adverse effects. Consider including studies that assess the impact of inhibitors or inducers of the cytochrome P450 system on prednisone metabolism.
Role of Gut Microbiome
Focus on the gut microbiome’s impact on prednisone metabolism and its subsequent effects on therapeutic efficacy. Emerging data suggests that gut bacteria can influence drug metabolism, opening avenues for probiotic interventions to optimize treatment. Clinical studies could assess the correlation between microbiome diversity and the pharmacokinetics of prednisone.