Monitor patients closely for symptoms of lidocaine toxicity, as rapid identification can prevent serious complications. Early signs typically manifest as central nervous system disturbances, including tingling or numbness around the mouth, as well as dizziness and visual disturbances.
Recognize these symptoms as the body’s response to elevated lidocaine levels. Prompt reporting is crucial; consider dosage adjustments or alternative medications if any of these signs occur. Conduct a thorough assessment to determine the patient’s medical history, current medications, and overall condition to identify potential risk factors.
Engage in constant communication with patients, encouraging them to report any unusual sensations or discomfort. This collaboration plays a key role in early detection. Maintain awareness of the maximum recommended dosage for lidocaine use, differentiating between infiltration, nerve block, and other administration methods to mitigate the likelihood of toxicity.
First Signs of Lidocaine Toxicity
Watch for initial symptoms of lidocaine toxicity, including confusion, dizziness, and tinnitus. These signs often present early and require immediate attention. Patients may experience a metallic taste, tingling sensations, or numbness around the mouth. Monitor for altered mental status, as this could indicate increasing levels of toxicity.
Neurological Symptoms
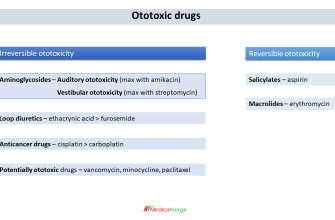
Neurological manifestations can escalate quickly. Look out for tremors, seizures, or loss of consciousness. It’s important to remain vigilant, as these symptoms may indicate that the patient is moving toward severe toxicity. Calculate the total dose administered and compare it with recommended dosage guidelines to assess the situation.
Cardiovascular Effects
Cardiovascular symptoms may follow, such as bradycardia or hypotension. Arrhythmias can also occur, which underline the necessity of continuous cardiac monitoring during the use of lidocaine. If any cardiovascular symptoms present alongside neurological signs, intervene immediately and be prepared to initiate resuscitation protocols if needed.
Identifying Initial Symptoms of Lidocaine Overdose
Recognizing the signs of lidocaine overdose quickly can prevent serious complications. The first symptoms often include central nervous system effects. Patients may experience dizziness, tinnitus (ringing in the ears), or visual disturbances. These symptoms indicate that lidocaine levels are rising excessive in the bloodstream.
Neurological Signs
Behavioral changes are common early indicators. Individuals might exhibit anxiety, agitation, or confusion. Increased restlessness along with paresthesia (tingling sensations) can manifest as well. Watch for these changes closely, as they may evolve into more severe neurological effects like seizures.
Cardiovascular Manifestations
Pay attention to cardiovascular symptoms, as they can escalate quickly. Initial signs include bradycardia (slowed heart rate) and hypotension (low blood pressure). Patients might report feelings of palpitations or irregular heartbeats. Monitor these vital signs continuously to detect worsening conditions.
Responding swiftly to any of these symptoms is essential. Immediate medical intervention can mitigate risks and enhance recovery outcomes. Proper assessment and dosing techniques help reduce the likelihood of overdose, ensuring patient safety during lidocaine administration.
Diagnostic Tools for Early Detection of Lidocaine Toxicity
Utilize point-of-care ultrasound to assess cardiac function and detect arrhythmias, an early indicator of lidocaine toxicity. This tool enables rapid evaluation of the heart’s contractility and rhythm irregularities, which can signal impending toxicity.
Capnography serves as another valuable diagnostic instrument. It monitors end-tidal carbon dioxide levels, providing insight into respiratory function and potential central nervous system effects from lidocaine. A rise in carbon dioxide may indicate respiratory depression, a warning sign of toxicity.
Routine ECG monitoring is vital. Look for changes in QRS duration or PR interval, as these abnormalities can indicate sodium channel blockade associated with lidocaine accumulation.
Serum lidocaine levels provide quantitative data on drug concentration in the bloodstream. Regularly testing these levels assists in identifying patients at risk for toxicity, especially in those receiving continuous infusions or with underlying liver dysfunction.
Clinical assessment scales, such as the McNicol criteria, help guide decision-making in suspected cases of toxicity. These scales evaluate the neurological status of the patient, highlighting symptoms such as dizziness, confusion, or seizures that may arise due to excessive lidocaine levels.
Lastly, always maintain a high index of suspicion for lidocaine toxicity in vulnerable populations, including those with hepatic impairment or cardiac conditions. Early recognition through these diagnostic tools ensures timely intervention and better outcomes.
Immediate Interventions for Suspected Lidocaine Toxicity
Remove the source of lidocaine immediately. Provide supplemental oxygen to support breathing. Establish intravenous access to facilitate rapid medication administration and fluid resuscitation.
If seizures occur, administer benzodiazepines such as lorazepam or midazolam. Monitor the patient’s airway continuously, and prepare for potential airway management if respiratory depression is evident. Assess circulatory status and initiate cardiopulmonary resuscitation (CPR) if there are signs of cardiac arrest.
- Establish vital signs monitoring.
- Perform a 12-lead ECG to identify dysrhythmias.
- Consider administering intralipid emulsion therapy if cardiovascular collapse develops.
Consult a toxicologist or a medical specialist for guidance on advanced management strategies. Stay vigilant for symptoms such as confusion, tinnitus, or seizures, which warrant immediate intervention.
Document all findings and interventions precisely. Ensure communication with emergency medical services if transport is necessary, providing a clear history of lidocaine exposure and interventions performed.