Prednisone and prednisolone are often discussed interchangeably, but they are not quite the same. Prednisone is a prodrug that the liver converts into prednisolone, its active form. This conversion process is essential for experiencing the medication’s therapeutic effects. For most patients, prednisolone is generally prescribed in situations where immediate action is necessary, such as in acute inflammation or severe allergic reactions.
In clinical practice, the choice between these medications can depend on several factors, including a patient’s specific health condition and how their body metabolizes prednisone. Those with liver issues may require prednisolone directly since their ability to convert prednisone is compromised. Always consult with a healthcare provider to determine which option is more suitable for your treatment plan.
The dosage forms may also differ. Prednisone is typically available in oral tablets, while prednisolone comes in various forms such as syrups, solutions, and tablets. These variations can offer flexibility in administration, especially for different age groups or medical conditions. Your healthcare provider can guide you on the most appropriate form for your situation.
Understanding the distinctions between prednisone and prednisolone enhances your knowledge about your treatment options. Make informed decisions by discussing both medications with your healthcare team to ensure you receive the best care tailored to your needs.
- Is Prednisone Same as Prednisolone?
- Understanding the Basics of Prednisone and Prednisolone
- Chemical Structure: Differences and Similarities
- Molecular Composition
- How Both Medications Work in the Body
- Mechanism of Action
- Effects on the Immune System
- Common Uses for Prednisone and Prednisolone
- 1. Allergic Reactions
- 2. Autoimmune Disorders
- 3. Respiratory Conditions
- 4. Organ Transplants
- 5. Certain Cancers
- Dosage Forms and Administration Routes
- Oral Administration
- Parenteral Administration
- Side Effects and Risks of Each Medication
- Prednisone
- Prednisolone
- Comparative Risks
- Monitoring and Management
- Drug Interactions to Be Aware Of
- Common Interactions
- Other Notable Interactions
- When to Choose Prednisone Over Prednisolone and Vice Versa
- Specific Indications
- Formulations and Administration
Is Prednisone Same as Prednisolone?
Prednisone and prednisolone are closely related medications, but they are not identical. Both belong to the category of corticosteroids and serve similar therapeutic purposes, such as reducing inflammation and suppressing the immune response.
Prednisone is a prodrug, meaning the body converts it into prednisolone after ingestion. Prednisolone is the active form, which means it acts directly on the body’s systems. This conversion makes the two drugs interchangeable in many situations, but some patients may respond differently to each formulation.
| Attribute | Prednisone | Prednisolone |
|---|---|---|
| Classification | Prodrug | Active form |
| Administration | Oral | Oral, injectable |
| Conversion | Converted in the liver | No conversion needed |
| Uses | Similar therapeutic uses | Similar therapeutic uses |
Consult a healthcare provider to determine which medication is best suited for your condition. Factors such as your health status, how your body metabolizes medications, and specific treatment goals play an important role in this decision.
Understanding the Basics of Prednisone and Prednisolone
Prednisone and prednisolone are corticosteroids that reduce inflammation and suppress the immune system. While both medications are used to treat similar conditions, it’s important to note that they differ slightly in structure and how they are metabolized in the body.
Prednisone is a prodrug, meaning it must be converted by the liver into prednisolone to become active. This conversion can be slower in individuals with liver impairment, making prednisolone the preferred choice in those cases. Prednisolone acts directly, leading to a more immediate effect.
Both medications are effective for conditions like asthma, allergies, and autoimmune disorders. The choice between them often depends on the patient’s specific needs and health conditions. For example, prednisolone may be prescribed for immediate action, while prednisone is frequently used for its easier availability in oral form.
Dosing may differ, and it’s crucial to follow a healthcare provider’s instructions carefully. Patients should also be aware of potential side effects, such as weight gain, increased blood sugar levels, and mood changes, which can occur with both medications.
Always consult a healthcare professional to determine the most suitable option for your situation, considering factors like health history, current medications, and any existing medical conditions.
Chemical Structure: Differences and Similarities
Prednisone and prednisolone possess similar chemical structures, as both are corticosteroids derived from the steroid hormone cortisol. Prednisone is a synthetic analogue that converts to prednisolone in the liver. This conversion is vital for its pharmacological activity, linking the two compounds closely in function and effect.
Molecular Composition
The molecular formula for both prednisone and prednisolone is C21H26O5. However, the key distinction lies in their configuration. Prednisone has a double bond between carbon atoms 1 and 2, while prednisolone contains a hydroxyl group at the 11-position, which allows it to exhibit a slightly altered pharmacodynamics. This modification affects their absorption and metabolic pathways.
Prednisone and prednisolone operate as corticosteroids, effectively lowering inflammation and suppressing the immune response. They mimic cortisol, a hormone produced by the adrenal glands, impacting various functions in the body.
Mechanism of Action
After ingestion, prednisone undergoes conversion in the liver to prednisolone, the active form. Both medications bind to glucocorticoid receptors in the cytoplasm of cells, altering gene expression. This process leads to the decreased production of inflammatory mediators such as cytokines and prostaglandins.
Effects on the Immune System
These medications specifically reduce the activity of white blood cells. This suppression helps in managing autoimmune conditions and allergies, providing relief from symptoms. Regular use may also influence metabolic processes, affecting glucose levels and fat distribution in the body.
Always consult with a healthcare provider regarding dosage and duration to avoid potential side effects. Regular monitoring can help maintain balance in the body’s response to inflammation and immune reactions.
Common Uses for Prednisone and Prednisolone
Prednisone and prednisolone serve multiple medical purposes due to their anti-inflammatory and immunosuppressive properties.
1. Allergic Reactions
Both medications effectively manage severe allergic responses, including:
- Asthma exacerbations
- Allergic rhinitis
- Skin reactions such as dermatitis or hives
2. Autoimmune Disorders
These corticosteroids reduce inflammation in various autoimmune conditions by modulating the immune response. Common uses include:
- Rheumatoid arthritis
- Lupus
- Multiple sclerosis
In addition, they play a crucial role in treating conditions such as:
- Inflammatory bowel diseases (like Crohn’s disease and ulcerative colitis)
- Psoriasis
3. Respiratory Conditions
Prednisone and prednisolone help alleviate symptoms of respiratory illnesses, particularly in cases of:
- Chronic obstructive pulmonary disease (COPD)
- Pneumonia
- Bronchitis
4. Organ Transplants
They are crucial in preventing rejection following organ transplants by suppressing the immune system to accept the new organ.
5. Certain Cancers
These medications can also treat specific types of cancer, including:
- Leukemia
- Lymphoma
In all cases, monitoring and adjusting dosages based on individual response is essential for safe and effective treatment. Always consult healthcare professionals for tailored medical advice.
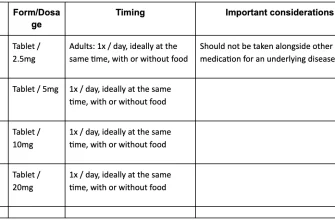
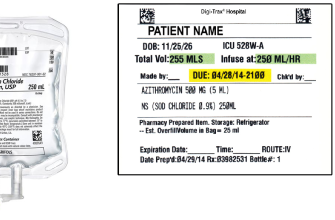
Dosage Forms and Administration Routes
Prednisone and prednisolone are available in several dosage forms and routes of administration. The most common forms include oral tablets, oral solutions, and injectable options. Each form provides flexibility depending on patient needs and specific medical conditions.
Oral Administration
Both medications are frequently prescribed as oral tablets, typically ranging from 1 mg to 50 mg. Patients should take these with food to minimize gastrointestinal irritation. Oral solutions provide an alternative for those who have difficulty swallowing tablets. Dosing can be adjusted based on individual requirements, often starting with a higher dose and tapering as needed.
Parenteral Administration
Injectable forms of prednisone and prednisolone cater to situations requiring rapid intervention, such as acute allergic reactions or adrenal insufficiency. These injections can be given intramuscularly or intravenously, depending on the urgency of the situation. It’s essential to follow the prescribed dosage and injection protocol for safety and efficacy.
Consult your healthcare provider to determine the most suitable dosage form and administration route for your particular condition.
Side Effects and Risks of Each Medication
Prednisone and prednisolone, while closely related, come with their own set of side effects and risks. Understanding these can guide treatment decisions effectively.
Prednisone
- Weight Gain: Patients may experience increased appetite and subsequent weight gain.
- Hypertension: Monitor blood pressure regularly as prednisone can elevate it.
- Blood Sugar Levels: This medication can cause elevated blood sugar, necessitating regular checks, especially for diabetics.
- Gastrointestinal Issues: Users might face stomach irritation, ulcers, or other digestive discomforts.
- Osteoporosis: Long-term use can weaken bones, increasing fracture risk.
- Immune Suppression: Be cautious of infections, as prednisone can lower immune response.
Prednisolone
- Similar Weight Gain: Like prednisone, it can enhance appetite leading to excess weight.
- Fluid Retention: Patients might notice swelling due to fluid retention.
- Hypertension: Regular monitoring of blood pressure is advised.
- Gastrointestinal Risks: Risk of gastritis and peptic ulcers remains significant.
- Mood Changes: Prednisolone can affect mood, causing irritability or depression.
- Skin Changes: Skin thinning and easy bruising may occur with extended use.
Comparative Risks
While both medications share many side effects, individual reactions may vary. Prednisone, often converted to prednisolone in the liver, may carry slightly different risk profiles based on individual metabolism and health status.
Monitoring and Management
- Regular Check-Ups: Ensure frequent follow-ups with healthcare providers to monitor side effects.
- Adjust Doses: Dosage adjustments may mitigate some risks; always consult with a doctor.
- Healthy Lifestyle: Engage in regular exercise and maintain a balanced diet to counteract weight gain and support overall health.
Awareness of potential side effects allows for proactive management, contributing to safer use of these medications. Always consult healthcare professionals before making any changes to medication regimens.
Drug Interactions to Be Aware Of
Pay close attention to potential drug interactions when using prednisone or prednisolone. Certain medications can alter the effectiveness or lead to adverse effects. Always consult your healthcare provider before starting or stopping any medication.
Common Interactions
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Combining these with corticosteroids increases the risk of gastrointestinal bleeding.
- Anticoagulants: Prednisone may affect the efficacy of blood thinners like warfarin, requiring careful monitoring of blood clotting parameters.
- Aspirin: Use with caution as it may heighten the possibility of gastrointestinal issues.
- Diuretics: Corticosteroids can influence potassium levels, so monitor electrolytes when taken concurrently with diuretics.
- Antidiabetic Medications: Corticosteroids may alter your blood sugar levels. Insulin or oral hypoglycemic agents might need adjustment.
Other Notable Interactions
- Vaccines: Live vaccines are not recommended during treatment due to the risk of infection.
- Antifungal Medications: Drugs such as ketoconazole can increase prednisone levels in the body, leading to enhanced effects.
- Anticonvulsants: Some may reduce the effectiveness of prednisone, requiring dosage adjustments.
Regularly review your medications with a healthcare provider to ensure safety and efficacy. Report any unexpected side effects promptly for appropriate management.
When to Choose Prednisone Over Prednisolone and Vice Versa
Choose prednisone for conditions requiring rapid action, especially if an oral form is needed and the patient has a particular need for a longer duration of effects. It is often preferred in acute situations or when immediate symptom relief is necessary. For instance, prednisone can be advantageous in cases of severe allergic reactions or exacerbations of chronic conditions like asthma.
Opt for prednisolone when treating patients with liver impairment or those unable to metabolize medications effectively. Prednisolone, a metabolite of prednisone, requires less conversion in the liver, making it a better choice for individuals facing hepatic issues. Always consider the patient’s metabolic capacity when making this choice.
Specific Indications
Prednisone is often indicated for conditions like autoimmune disorders, post-transplant management, or specific cancers. Its properties make it suitable for reducing inflammation and managing immune responses swiftly. Conversely, prednisolone is frequently prescribed to children due to its safety profile and bioavailability, especially for conditions like asthma and certain hematological disorders.
Formulations and Administration
Preferred formulations play a significant role in your decision. If intravenous administration is required, consider using prednisolone as it may be more effective in certain acute scenarios. Both medications come in various forms, but the choice may depend on the patient’s specific needs, such as ease of administration or patient compliance.
Evaluate each situation based on the patient’s overall health, response to previous treatments, and potential drug interactions. Make informed decisions by assessing the unique circumstances surrounding each case for optimal management.