For patients with chronic kidney disease (CKD), Lasix (furosemide) can play a significant role in managing symptoms related to fluid overload. Administering Lasix helps to effectively reduce excess fluid retention, alleviating symptoms such as edema and hypertension. An appropriate dosage is crucial, typically ranging from 20 mg to 80 mg daily, depending on individual patient needs and medical advice.
Regular monitoring of renal function and electrolytes is essential while on Lasix. Hyperkalemia and dehydration are potential side effects that require vigilance. Adjustments to the dosage may be necessary based on urine output and kidney function tests. Engaging with healthcare providers ensures that the treatment plan remains tailored to the patient’s evolving health status.
Combining Lasix with a sodium-restricted diet can enhance its effectiveness. Patients should monitor their fluid intake and work with nutritionists to maintain a balanced diet that supports kidney health. By prioritizing these strategies, individuals with CKD can better manage their condition and improve their overall quality of life.
- Lasix for Chronic Kidney Disease
- Understanding Chronic Kidney Disease and Its Symptoms
- How Lasix Works in the Treatment of CKD
- Dosage Guidelines for Lasix in CKD Patients
- Adjusting Dosage
- Frequency of Administration
- Side Effects and Risks of Using Lasix
- Monitoring Kidney Function While on Lasix
- Key Parameters to Monitor
- Symptoms to Watch For
- Dietary Considerations When Taking Lasix
- Potassium Management
- Stay Hydrated
- Drug Interactions with Lasix in CKD Management
- Patient Experiences and Case Studies with Lasix
- Patient Feedback on Dosage and Side Effects
- Table of Patient Outcomes with Lasix
Lasix for Chronic Kidney Disease
Lasix, or furosemide, is commonly prescribed for managing fluid retention in patients with chronic kidney disease (CKD). It works by promoting diuresis, aiding in the removal of excess fluid from the body. This is particularly beneficial for patients experiencing edema, which can result from impaired kidney function.
Dosage typically begins at 20 to 40 mg daily, adjusted based on the individual’s response and degree of fluid retention. Monitoring electrolytes is essential, as Lasix can lead to imbalances, especially in potassium and sodium levels. Regular blood tests should inform dosage adjustments to maintain electrolyte balance while effectively managing symptoms.
Patients should be cautious about potential side effects, including dehydration and hypotension. Staying well-hydrated and adhering to dietary recommendations can minimize these risks. Low-sodium diets and potassium-rich foods might be advised to support overall kidney health.
Consult healthcare providers regularly to assess kidney function and the effectiveness of Lasix therapy. Regular follow-ups enable timely modifications to treatment plans, optimizing health outcomes in chronic kidney disease management.
Understanding Chronic Kidney Disease and Its Symptoms
Recognizing symptoms of chronic kidney disease (CKD) allows for earlier intervention and management. CKD often progresses silently, making awareness of symptoms critical. Patients may notice fatigue, swelling in the legs or ankles, changes in urination patterns, and persistent high blood pressure.
Common symptoms include:
| Symptom | Description |
|---|---|
| Fatigue | A feeling of constant tiredness due to reduced red blood cell production. |
| Swelling | Fluid retention causing puffiness, primarily in legs and ankles. |
| Urination Changes | Increased frequency; darker urine; foamy urine indicating protein loss. |
| High Blood Pressure | Elevated levels worsen kidney function and require regular monitoring. |
Weight loss and poor appetite may emerge as CKD advances, leading to nutritional deficiencies. Patients might also experience itchy skin and muscle cramps. Cognitive changes, such as difficulty concentrating, can also occur due to toxin buildup in the body.
Engaging with healthcare providers for routine screening and comprehensive evaluations is essential. Regular monitoring can help manage symptoms and slow disease progression, ultimately supporting better health outcomes for those affected by chronic kidney disease.
How Lasix Works in the Treatment of CKD
Lasix, also known as furosemide, serves a specific role in managing chronic kidney disease (CKD). This diuretic primarily works by inhibiting sodium and chloride reabsorption in the loop of Henle, a crucial part of the nephron. This mechanism leads to increased urine output, aiding in the reduction of fluid overload associated with CKD.
By promoting diuresis, Lasix helps to decrease blood volume, which can alleviate hypertension and reduce the burden on the kidneys. Patients with CKD often experience fluid retention, and Lasix effectively addresses this symptom, improving comfort and quality of life.
Careful monitoring of electrolyte levels is essential when using Lasix, as the drug can lead to imbalances, particularly of potassium and magnesium. Regular blood tests allow healthcare providers to adjust dosages accordingly, ensuring safe and effective treatment.
The timing of administration is vital. Taking Lasix in the morning helps prevent nocturia, allowing patients a better night’s sleep. Increasing fluid intake can mitigate some electrolyte disturbances; however, this must be balanced with the patient’s overall kidney function status.
Lasix plays a pivotal role in preventing complications related to fluid overload, such as heart failure. Combining diuretic therapy with other medications may enhance overall management of CKD. Collaboration between patients and healthcare providers fosters an effective treatment plan tailored to individual needs.
Dosage Guidelines for Lasix in CKD Patients
Lasix (furosemide) dosing in patients with chronic kidney disease (CKD) should start with lower doses to minimize the risk of adverse effects. Typically, initiate treatment with 20-40 mg once daily.
Adjusting Dosage
Monitor the patient’s response closely. If the desired diuresis is not achieved, consider the following adjustments:
- Increase the dose by 20 mg increments, with maximum doses up to 80 mg daily, based on clinical response.
- For patients with more advanced CKD (Stage 3-5), initiate with smaller doses, like 10 mg, and titrate gradually.
Frequency of Administration
In cases where higher doses are necessary, bifurcate the daily dose to twice daily administration to maintain effective diuretic action:
- For example, administering 40 mg in the morning and 40 mg in the evening.
Always adjust dosages based on renal function. Regularly monitor kidney function and electrolytes to avoid complications such as dehydration or electrolyte imbalances. Keep healthcare providers informed about any side effects or concerns during treatment.
Side Effects and Risks of Using Lasix
Lasix (furosemide) can help manage fluid retention in chronic kidney disease, but it comes with potential side effects and risks. Understanding these can aid in safer use and effective monitoring.
- Electrolyte Imbalance: Lasix can lead to low potassium (hypokalemia) and magnesium levels. Regular blood tests are recommended to monitor these electrolytes.
- Dehydration: Excessive diuresis may result in dehydration, leading to dizziness, dry mouth, or increased thirst. Maintain adequate fluid intake unless otherwise directed by a healthcare provider.
- Kidney Function: In some cases, Lasix can worsen kidney function. Regular assessments of renal function are crucial to detect any decline early.
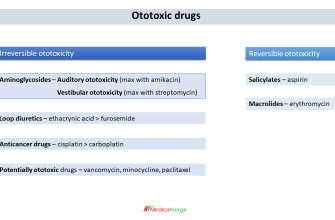
- Ototoxicity: High doses or rapid intravenous administration may cause hearing disturbances. Patients should report any changes in hearing immediately.
- Allergic Reactions: Skin rashes, itching, or other allergic symptoms can occur. If any signs of allergy appear, consult a healthcare professional promptly.
Patients should engage in open communication with their healthcare team about any side effects experienced. This information plays a key role in managing dosages effectively and adjusting treatment as needed.
- Interactions: Be aware of medications that may interact with Lasix, such as certain antihypertensives and steroids. Review all medications with a healthcare provider.
- Regular Monitoring: Schedule regular follow-ups to assess response to treatment and any emerging side effects.
By staying informed and proactive, patients can reduce the risks associated with Lasix while benefiting from its therapeutic effects.
Monitoring Kidney Function While on Lasix
Regular assessment of kidney function is critical for patients taking Lasix. Schedule kidney function tests every 3 to 6 months, depending on the presence of other health issues. Consider including serum creatinine, blood urea nitrogen (BUN), and electrolyte levels in these evaluations.
Key Parameters to Monitor
- Serum Creatinine: Track levels to detect any decline in kidney function. An increase may indicate worsening kidney status.
- BUN: Monitor BUN levels, as elevated levels can also reflect kidney impairment.
- Electrolytes: Pay close attention to potassium, sodium, and magnesium to prevent imbalances caused by Lasix.
- Urinalysis: Conduct urinalysis to identify changes in protein levels or the presence of blood, indicating potential issues.
Symptoms to Watch For
Be alert for symptoms that may signal declining kidney function while on Lasix:
- Increased swelling in extremities
- Unusual fatigue or weakness
- Changes in urine output
- Elevated blood pressure readings
If any concerning symptoms arise or abnormal lab results occur, adjust the dosage or consider alternative therapies under medical supervision. Staying proactive ensures optimal management of kidney function while benefiting from Lasix treatment.
Dietary Considerations When Taking Lasix
Limit sodium intake to help manage fluid retention caused by Lasix. Aim for less than 2,300 mg of sodium per day, or a lower amount if recommended by your healthcare provider. This will support the medication’s effectiveness and reduce the risk of high blood pressure.
Potassium Management
Monitor potassium levels closely. Lasix can lead to low potassium, a condition known as hypokalemia. Incorporate potassium-rich foods such as bananas, oranges, and spinach into your diet, unless your doctor advises otherwise. Regular blood tests can help track your potassium status.
Stay Hydrated
Maintain adequate hydration. While Lasix promotes fluid excretion, drinking enough water is crucial to prevent dehydration. Balance fluid intake with your doctor’s guidelines, especially if you have conditions that require fluid restrictions.
Drug Interactions with Lasix in CKD Management
Monitor potassium levels closely when prescribing Lasix, especially in patients already on potassium-depleting medications such as thiazide diuretics or certain antihypertensives. Combining these agents can lead to significant hypokalemia, increasing the risk of cardiac complications.
Watch for interactions with NSAIDs, which can reduce the effectiveness of Lasix by promoting sodium and water retention. Advise patients to limit NSAID use, particularly during renal impairment periods.
Caution is advised when administering Lasix alongside aminoglycosides, as both can heighten the risk of nephrotoxicity. Consider alternative antibiotics when possible, and monitor renal function closely.
Assess digoxin therapy concurrently with Lasix. Diuretic-induced potassium depletion can magnify digoxin’s effects, raising the risk of toxicity. Regularly check serum levels of both drugs in patients taking them together.
Be aware of the interaction between Lasix and certain antidepressants, like SSRIs. These medications may also impact sodium balance and fluid status, increasing the potential for electrolyte disturbances.
Educate patients regarding the signs of dehydration and electrolyte imbalance, since polypharmacy can complicate these aspects.
Adjust dosages accordingly based on renal function. In CKD patients, Lasix dosages may need modification to avoid exacerbating existing renal issues. Regularly review laboratory values to help guide treatment decisions.
Consider implications of combining Lasix with other diuretics. The interaction may produce an additive effect, leading to excessive diuresis and potential renal impairment. Use these combinations judiciously.
Evaluate blood pressure medications in the context of Lasix use. Certain antihypertensives can have additive effects but may also increase dehydration risks. Tailor treatment regimens for optimal outcomes.
Provide continuous education to patients about their medications and potential interactions with Lasix. Empower them to communicate any changes or concerns with their healthcare provider.
Patient Experiences and Case Studies with Lasix
Patients with chronic kidney disease (CKD) often share positive outcomes when using Lasix (furosemide) as part of their treatment regimen. Many report significant improvements in fluid management and overall comfort. For instance, a patient diagnosed with stage 3 CKD noticed a substantial decrease in swelling after incorporating Lasix into their daily routine. This medication helped them maintain a more balanced fluid status, alleviating discomfort during daily activities.
Case studies highlight the drug’s role in managing symptoms effectively. One 62-year-old male patient presented with hypertension and fluid overload. After starting Lasix at a low dose, his blood pressure stabilized, and he reduced his weight by 5 kg in just a few weeks. He experienced fewer hospitalizations due to better fluid control.
Patient Feedback on Dosage and Side Effects
Many patients adapt well to Lasix, but individual responses vary. Some individuals report mild side effects such as dizziness or electrolyte imbalances, which often resolve with dosage adjustments. Regular monitoring helps mitigate these concerns. A patient experienced mild potassium depletion and worked with their healthcare provider to include potassium-rich foods in their diet, improving their overall well-being.
Table of Patient Outcomes with Lasix
| Patient Profile | Initial Condition | Lasix Dose | Outcome |
|---|---|---|---|
| 62-year-old Male | Stage 3 CKD, Hypertension | 20 mg | Weight loss of 5 kg, stabilized blood pressure |
| 58-year-old Female | Fluid Overload | 40 mg | Reduced swelling, improved daily comfort |
| 70-year-old Male | Heart Failure with CKD | 80 mg | Enhanced mobility, fewer hospital admissions |
Patient experiences demonstrate that with careful management, Lasix can significantly enhance quality of life for individuals with CKD. Tailoring therapy to individual needs ensures optimal results while minimizing potential side effects. Regular follow-ups and open communication with healthcare providers remain key to successful treatment outcomes.