If you notice a rash developing on your face while taking prednisone, it’s important to address it promptly. Identifying the symptoms often helps in understanding the underlying causes and deciding on the best course of action. Common signs of prednisone-induced rash include redness, irritation, and potential peeling of the skin.
Start by consulting your healthcare provider before making any changes to your medication. They might recommend adjusting the dosage or switching to an alternative treatment that doesn’t cause skin reactions. Meanwhile, maintain a gentle skincare routine; opt for mild cleansers and moisturizers that soothe irritation and avoid products with harsh chemicals or fragrances.
Applying cool compresses can help reduce inflammation and discomfort. If the rash persists or worsens, your doctor may suggest topical corticosteroids to ease symptoms. Stay hydrated and follow a balanced diet rich in vitamins to support your skin’s healing process. Regular follow-ups with your healthcare provider will ensure you effectively manage any changes in your skin condition while on prednisone.
- Understanding Prednisone Rash on Face
- What is Prednisone and Its Common Uses?
- Identifying Prednisone-Induced Rash Symptoms
- Causes of Facial Rash While Taking Prednisone
- When to Seek Medical Attention for Rash
- Effective Treatment Options for Prednisone Rash
- Preventive Measures to Avoid Facial Rash on Prednisone
- Alternative Medications to Consider if Rash Occurs
- Long-Term Effects of Prednisone on Skin Health
- Increased Susceptibility to Infections
- Changes in Pigmentation
Understanding Prednisone Rash on Face
Prednisone can trigger facial rashes in some individuals, often presenting as redness, swelling, or bumps. Identifying this reaction early helps manage symptoms effectively. If you notice unusual changes on your face after starting prednisone, consult your healthcare provider to discuss your symptoms and possible alternatives.
To alleviate discomfort, consider using gentle skincare products. Choose hypoallergenic and fragrance-free options to avoid further irritation. Moisturizers can help soothe the skin, while cool compresses may reduce swelling and redness.
Avoid exposure to harsh sunlight, as prednisone can increase skin sensitivity. Use sunscreen daily, even on cloudy days, to protect your skin. Wearing a wide-brimmed hat when outside also provides an extra layer of protection.
Diet plays a role in skin health too. Incorporating anti-inflammatory foods, such as fruits, vegetables, and omega-3 rich items like fish, may support your skin. Staying hydrated helps maintain skin elasticity and overall health.
If the rash persists or worsens, your doctor may recommend medications to manage the symptoms. Topical corticosteroids or antihistamines can be effective treatments. Always follow your healthcare provider’s instructions for application and dosage.
Keeping track of any other medications you’re taking is essential, as interactions may exacerbate rashes. Maintaining open communication with your healthcare team ensures safe and effective management of your skin condition.
Lastly, engaging in stress-reducing activities, such as yoga or meditation, can help your skin by improving overall well-being. Stress management is key, as heightened stress levels can impact skin reactions.
What is Prednisone and Its Common Uses?
Prednisone is a synthetic corticosteroid that mimics the effects of hormones produced by the adrenal glands. It works by suppressing the immune response and reducing inflammation in the body.
Healthcare providers commonly prescribe prednisone for a variety of conditions, including:
- Allergic reactions: Effective for treating severe allergies and skin reactions.
- Autoimmune diseases: Manages symptoms of diseases like lupus and rheumatoid arthritis.
- Respiratory conditions: Alleviates symptoms of asthma and chronic obstructive pulmonary disease (COPD).
- Inflammatory disorders: Used for conditions such as inflammatory bowel disease and dermatitis.
- Organ transplant: Prevents rejection by suppressing the immune system.
Although prednisone can be highly beneficial, it is vital to follow a healthcare provider’s instructions regarding dosage and duration to minimize potential side effects. Monitoring is essential, particularly for long-term use, as this medication can affect various bodily systems.
Quickly addressing any side effects, such as skin rashes or mood changes, enhances the management of your health while on prednisone. Regular check-ups can help ensure that you stay on track with your treatment plan.
Identifying Prednisone-Induced Rash Symptoms
Look for redness and swelling on the face, often accompanied by a bumpy texture. The rash may appear as small, raised red spots or patches, which can lead to dryness and flaking of the skin. Pay attention to itchiness or burning sensations, as these symptoms frequently occur with the rash.
Monitor for any changes in skin pigmentation, as prednisone can sometimes cause darkening or lightening in certain areas. Additionally, a rash may develop in areas where the skin folds, such as around the nose or under the eyes, making it essential to maintain awareness of these locations.
If you notice pus-filled blisters or an extensive spread of the rash, seek medical advice immediately. This may indicate a more serious reaction requiring prompt attention. Keep track of the duration; if the rash persists or worsens after discontinuing prednisone, consult a healthcare professional for further evaluation.
Consider keeping a log of your symptoms and any other medications or treatments you use alongside prednisone. This record may help your healthcare provider identify potential triggers or alternative solutions.
Causes of Facial Rash While Taking Prednisone
Facial rashes during prednisone treatment often stem from several factors. One of the primary causes is the immunosuppressive nature of prednisone. This medication dampens your immune response, making the skin more susceptible to infections, which can lead to rashes.
Allergic reactions can also trigger rashes. Some individuals might experience sensitivity to prednisone or other medications taken alongside it. Check ingredient labels and discuss any concerns with your healthcare provider.
Hormonal changes resulting from prednisone usage may disrupt skin balance, contributing to acne or other rashes. This is particularly prevalent among patients on long-term therapy. Maintaining a consistent skincare routine can help alleviate some of these effects.
Environmental factors play a role too. Prednisone can make skin thinner and more fragile, increasing vulnerability to irritants, such as harsh soaps or extreme temperatures. Use gentle, hypoallergenic products to minimize irritation.
Finally, underlying conditions may become more pronounced while on prednisone. Conditions like rosacea or eczema may flare up, causing facial rashes. Regular monitoring and communication with your dermatologist can help manage these conditions effectively.
When to Seek Medical Attention for Rash
If you experience a rash on your face while taking prednisone, monitor its characteristics closely. Seek medical help if the rash is widespread, persistent, or worsening over time. Pay attention to accompanying symptoms such as swelling, pain, or fever, which could indicate a more serious condition.
If the rash causes significant discomfort, itching, or affects your ability to perform daily activities, consider contacting a healthcare professional. Urgent intervention is necessary if you notice signs of an allergic reaction, such as difficulty breathing, hives, or swelling of the lips or throat.
It’s wise to seek guidance if the rash changes color, develops blisters, or shows signs of infection, such as warmth or drainage. These changes may warrant immediate evaluation to prevent complications.
Stay vigilant about any new symptoms that arise, as they may indicate a need for professional assessment. If you have underlying health conditions or take multiple medications, consult your doctor for personalized advice regarding any skin reactions.
Effective Treatment Options for Prednisone Rash
Topical corticosteroids significantly reduce inflammation associated with prednisone rash. Apply them sparingly to affected areas for swift relief.
Hydrocortisone cream is a common choice. Use 1% strength for mild cases a few times daily. In more severe reactions, a stronger prescription may be necessary, but consult a healthcare provider for guidance.
Moisturizers improve skin barrier function and alleviate dryness. Choose fragrance-free products to avoid further irritation. Apply after washing your face to lock in moisture.
Oral antihistamines, like cetirizine or diphenhydramine, help manage itching. Take these at night to improve sleep quality, especially if itching disrupts rest.
Avoid triggers that worsen rashes. Limit sun exposure, as UV rays can aggravate sensitive skin. Always use a broad-spectrum sunscreen with SPF 30 or higher when going outside.
Maintaining a gentle skincare routine is key. Use a mild cleanser and avoid harsh exfoliants or scrubs. Be cautious with new products; patch test before full application.
In cases of persistent or severe rash, discuss alternative medications with a healthcare professional. Sometimes, switching medications can provide a better outcome without triggering skin issues.
| Treatment Option | Usage Instructions |
|---|---|
| Topical Corticosteroids | Apply to affected areas as directed for inflammation |
| Hydrocortisone Cream | Use 1% strength for mild cases a few times daily |
| Moisturizers | Apply fragrance-free products after washing |
| Oral Antihistamines | Take to manage itching, preferably at night |
| Gentle Skincare | Use mild cleansers, avoid harsh products |
Regular follow-up with a dermatologist can help monitor the rash and adjust treatments as necessary. Address any concerns early to prevent worsening skin conditions.
Preventive Measures to Avoid Facial Rash on Prednisone
Keep your skin hydrated by applying a gentle, fragrance-free moisturizer daily. Look for products containing ceramides or hyaluronic acid to help maintain the skin barrier.
Avoid sun exposure by using a broad-spectrum sunscreen with at least SPF 30. Reapply every two hours, especially if you spend time outdoors.
Choose mild, non-comedogenic cleansers to wash your face. Avoid harsh scrubs and strong exfoliants that can irritate the skin further.
Monitor your diet and stay hydrated. Incorporate more fruits, vegetables, and omega-3 fatty acids to support skin health while limiting processed foods and sugars.
Apply makeup sparingly. Opt for mineral-based makeup products that are less likely to clog pores and cause irritation. Always remove makeup thoroughly before bedtime.
Consult your healthcare provider if you experience persistent rashes. They may adjust your prednisone dosage or recommend topical treatments to alleviate symptoms.
Avoiding known allergens and irritants, such as certain fabrics and fragrances, can help reduce the risk of a rash.
Practice stress management techniques. Stress can exacerbate skin conditions, so incorporate activities like yoga, meditation, or regular exercise into your routine.
Alternative Medications to Consider if Rash Occurs
If you experience a rash while using prednisone, consider these alternative medications:
- Hydrocortisone Cream: A mild topical steroid that helps reduce inflammation and soothe irritated skin. Apply a thin layer to the affected area as needed.
- Calamine Lotion: This soothing lotion can alleviate itching and discomfort. It’s especially effective for rashes that are itchy and uncomfortable.
- Antihistamines: Oral medications such as diphenhydramine or cetirizine can help control allergic reactions that may cause rashes. They work by blocking histamine, reducing itchiness and inflammation.
- Topical Immunomodulators: Medications like tacrolimus or pimecrolimus can be effective for inflammatory skin conditions. They help modulate the immune response and reduce skin irritation without the side effects of steroids.
- Other Steroids: If the rash persists, your doctor may suggest switching to a different corticosteroid, such as prednisolone or dexamethasone, which might offer a more suitable side effect profile for your condition.
Always consult with a healthcare professional before making changes to your medication regimen. They can provide tailored advice based on your specific situation.
Monitor your symptoms closely. If the rash worsens or you develop additional symptoms, seek medical attention promptly.
Long-Term Effects of Prednisone on Skin Health
Long-term use of prednisone can lead to several skin-related effects that require attention. Users often experience thinning skin, which increases vulnerability to bruising and tears. This phenomenon occurs because prednisone reduces collagen production, a crucial element for skin elasticity and strength.
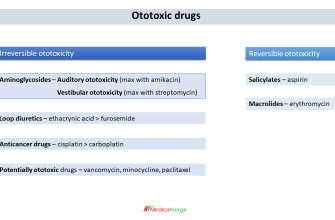
Increased Susceptibility to Infections
Chronic use of prednisone can impair the skin’s natural barrier, making it more susceptible to infections. Corticosteroids can alter the immune response, which may result in skin conditions like bacterial or fungal infections. Regular monitoring and prompt treatment of any skin infections are advisable to prevent complications.
Changes in Pigmentation
Users may notice changes in skin pigmentation over time. This can manifest as darkened patches or lighter areas on the skin. Regular moisturizing and sun protection can help manage these changes and keep the skin healthy. Consult a dermatologist for targeted treatments to address pigmentation issues if they arise.