When considering the conversion from Solumedrol (methylprednisolone) to prednisone, the typical equivalence is approximately 4 mg of Solumedrol for every 5 mg of prednisone. This means that if you are prescribed 40 mg of prednisone, the equivalent dose of Solumedrol would be around 32 mg. Understanding these ratios is vital for maintaining effective treatment while minimizing potential side effects.
Healthcare providers often rely on this conversion to ensure patients receive appropriate doses during corticosteroid therapy. Methylprednisolone has a shorter half-life compared to prednisone, impacting the frequency and timing of administration. It’s common to see Solumedrol given as an intravenous therapy in acute settings, making quick adjustments necessary for patient care.
Monitoring for adverse reactions becomes even more critical during transitions between these medications. Both drugs share similar side effects, including weight gain, mood changes, and increased blood sugar levels. Awareness of how these medications interact can lead to better patient outcomes and smoother treatment protocols.
Consult with your healthcare provider to determine the best course of action, as individual health circumstances and responses to medication are paramount in the treatment process.
- Understanding the Solumedrol to Prednisone Equivalent
- Dosage Formulations and Administration
- Clinical Considerations
- Dosage Conversion Between Solumedrol and Prednisone
- Clinical Considerations for Switching from Solumedrol to Prednisone
- Potential Side Effects of Solumedrol and Prednisone Comparison
- Patient Case Studies: Solumedrol vs. Prednisone Effectiveness
Understanding the Solumedrol to Prednisone Equivalent
In clinical practice, converting from Solumedrol (methylprednisolone) to prednisone requires careful dosage consideration. A common equivalence is that 4 mg of Solumedrol is roughly equal to 5 mg of prednisone. This means that if a patient is receiving 32 mg of Solumedrol per day, the equivalent dose of prednisone would be approximately 40 mg per day.
Dosage Formulations and Administration
Solumedrol is typically administered intravenously, while prednisone is taken orally. This difference in administration affects the onset of action. Solumedrol acts more rapidly due to intravenous delivery, making it suitable for acute conditions. When switching to prednisone, be mindful of the transition period and adjust for the slower onset of action with the oral formulation.
Clinical Considerations
Monitor patients closely during the switch to address any potential side effects or withdrawal symptoms. Tapering the dose is often necessary, especially if the patient has been on high doses of corticosteroids for an extended period. Always review the patient’s overall health status and specific condition before making any adjustments to their medication regimen.
Dosage Conversion Between Solumedrol and Prednisone
When converting from Solumedrol (methylprednisolone) to prednisone, a common equivalency is that 4 mg of Solumedrol is approximately equal to 5 mg of prednisone. For example, if a patient is prescribed 32 mg of Solumedrol, you can convert that to prednisone by calculating the equivalent dose as follows: 32 mg of Solumedrol corresponds to 40 mg of prednisone.
Carefully consider the condition being treated and the patient’s response to therapy when making dosage adjustments. Individual responses may vary, and it’s essential to monitor the patient for any potential side effects or required adjustments in dosage during the conversion process.
During the transition, maintain regular communication with the patient. Track their symptoms and overall well-being to ensure the new regimen is effective. If side effects from either medication arise, reassess and adjust the dosing strategy as needed.
Always involve the healthcare team in these conversions for the best patient outcomes. Customizing treatment based on specific needs will enhance safety and efficacy significantly.
Clinical Considerations for Switching from Solumedrol to Prednisone
Always assess the patient’s clinical status before making the switch from Solumedrol to prednisone. Monitor the dosage carefully; since Solumedrol is typically administered intravenously, converting to an oral formulation necessitates adjusting the dose accordingly.
- Calculate the equivalent oral dose of prednisone based on Solumedrol’s dosage. A common conversion ratio is 1 mg of Solumedrol to approximately 4 mg of prednisone.
- Evaluate the duration of steroid therapy. Longer durations may require a more gradual taper to minimize withdrawal symptoms.
- Consider the patient’s previous response to glucocorticoids. Any history of side effects from either medication should influence the decision.
- Monitor for signs of adrenal insufficiency, especially if transitioning from high-dose Solumedrol.
Set a clear tapering schedule for prednisone if the patient has been on a high dose of Solumedrol. Adjust based on therapeutic response and side effects.
Instruct the patient on possible side effects associated with prednisone, including weight gain, increased blood sugar levels, and mood changes. Provide guidance on lifestyle modifications to mitigate these effects.
- Advise regularly scheduled follow-ups to assess the effectiveness of the treatment and make adjustments as necessary.
- Review the patient’s other medications for potential interactions with prednisone.
Retain open communication with the patient throughout the switching process. This allows for timely identification of any adverse effects or therapeutic concerns, ensuring optimal care.
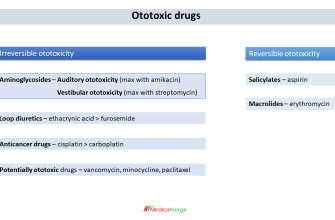
Potential Side Effects of Solumedrol and Prednisone Comparison
Both Solumedrol and prednisone can lead to similar side effects, but their intensity and likelihood may vary. Solumedrol, usually administered intravenously, often results in immediate effects, while prednisone typically requires oral administration and cumulative exposure before side effects become evident.
Common side effects for both medications include weight gain, mood changes, and elevated blood sugar levels. Patients using Solumedrol might experience more pronounced mood swings and euphoria due to its rapid delivery into the bloodstream. Prednisone users often report gradual changes in mood and sleep disturbances, which may be less intense initially.
Gastrointestinal issues are significant. Both medications can cause stomach upset, but Solumedrol may present a higher risk of acute gastrointestinal irritation due to its administration route. Patients on prednisone should take the medication with food to mitigate stomach issues.
Long-term use poses risks like osteoporosis and adrenal suppression for both drugs. However, Solumedrol’s potential for causing immediate immunosuppression necessitates careful monitoring during and post-treatment, especially in patients with pre-existing conditions.
Weight gain is a concern, with Solumedrol potentially causing faster accumulation due to its high potency. Prednisone-related weight gain can be more gradual, tied to duration and dosage. Both medications can lead to fat redistribution, particularly around the face and abdomen.
Sleep disturbances present an issue for many users. Solumedrol may lead to insomnia more quickly, likely due to its immediate effects on metabolism and mood. Prednisone may disturb sleep patterns over time as the body adjusts to its cumulative effects.
Consulting a healthcare provider for personalized advice regarding management and monitoring of side effects is vital. Regular assessments can help detect and address any concerns early, ensuring safer and more effective treatment strategies.
Patient Case Studies: Solumedrol vs. Prednisone Effectiveness
Patients diagnosed with autoimmune conditions often receive corticosteroids to manage inflammation. In a comparative review of Solumedrol (methylprednisolone) and prednisone, we observe varying responses that guide treatment choices.
In one case, a 52-year-old female with severe rheumatoid arthritis transitioned from prednisone to Solumedrol. Initial prednisone treatment (40 mg/day) improved her symptoms, but the side effects, including weight gain and mood swings, became problematic. Switching to Solumedrol (80 mg via IV weekly) resulted in quicker symptom relief and minimal side effects, highlighting Solumedrol’s potency in short-term management.
Another patient, a 35-year-old male with chronic asthma, was treated with prednisone (60 mg/day) during exacerbations. While effective, he experienced significant insomnia and increased appetite. After shifting to Solumedrol (125 mg IV formulation during acute attacks), his symptoms improved without the adverse effects associated with long-term prednisone use.
| Patient | Condition | Initial Treatment | Outcome |
|---|---|---|---|
| 52-year-old female | Rheumatoid arthritis | Prednisone (40 mg/day) | Improvement but significant side effects; switched to Solumedrol |
| 35-year-old male | Chronic asthma | Prednisone (60 mg/day) | Effectiveness was noted, but sleep disturbance led to change; switched to Solumedrol |
A third study reports on a 40-year-old female with multiple sclerosis. She utilized oral prednisone (30 mg/day), finding it insufficient during flare-ups. Intravenous Solumedrol (500 mg for 3 days) provided rapid control of her symptoms, demonstrating its advantage in acute settings.
Clinicians should consider individual patient profiles–responses to medication can vary widely. Solumedrol often shows quicker action and tolerance than prednisone, particularly in acute situations or when high dosages are necessary. Monitoring dosage and patient feedback remains key in determining the optimal therapy path.